At the end of DeOnte Taylor’s recent shift, only one bed remained. The respiratory therapist says his hospital in Oakland was lucky that two critically ill patients didn’t arrive at the same time.
“We’ve been barely missing capsizing,” Taylor said.
He fears the surge will topple the facility by the end of the week.
“I think it’s going to be chaotic. Only severe patients will be admitted … because we can only take care of the worst,” he said.
That’s also the reality unfolding at Kaiser Permanente’s Fresno Medical Center. Nurses struggle to fit inside rooms where two beds have been shoved inside. Staff are scrambling to convert conference rooms and a cafeteria into care facilities.
“We are at the point where we are having to triage who deserves an ICU bed and who doesn’t,” said registered nurse Amy Arlund at the end of a harrowing night shift. “We have to look at the severity of each patient and evaluate the chances of survival and pick the best candidate for a bed.”
Arlund says many hospitals in Fresno are beyond capacity. Across California, 80% of the intensive care units are full, according to Carmela Coyle, president and CEO of the California Hospital Association. San Diego, Los Angeles, Imperial County and the entire San Joaquin Valley are the worst hot spots, she said. But, she stressed, Northern California is not going to dodge this particular bullet this time.
Sunday’s single-day tally of 30,000 positive COVID-19 tests in California is three times higher than the total any day during the summer peak. A record-breaking 11,000 people across the state are lying in a hospital bed fighting the virus, an 87% increase over the last two weeks.
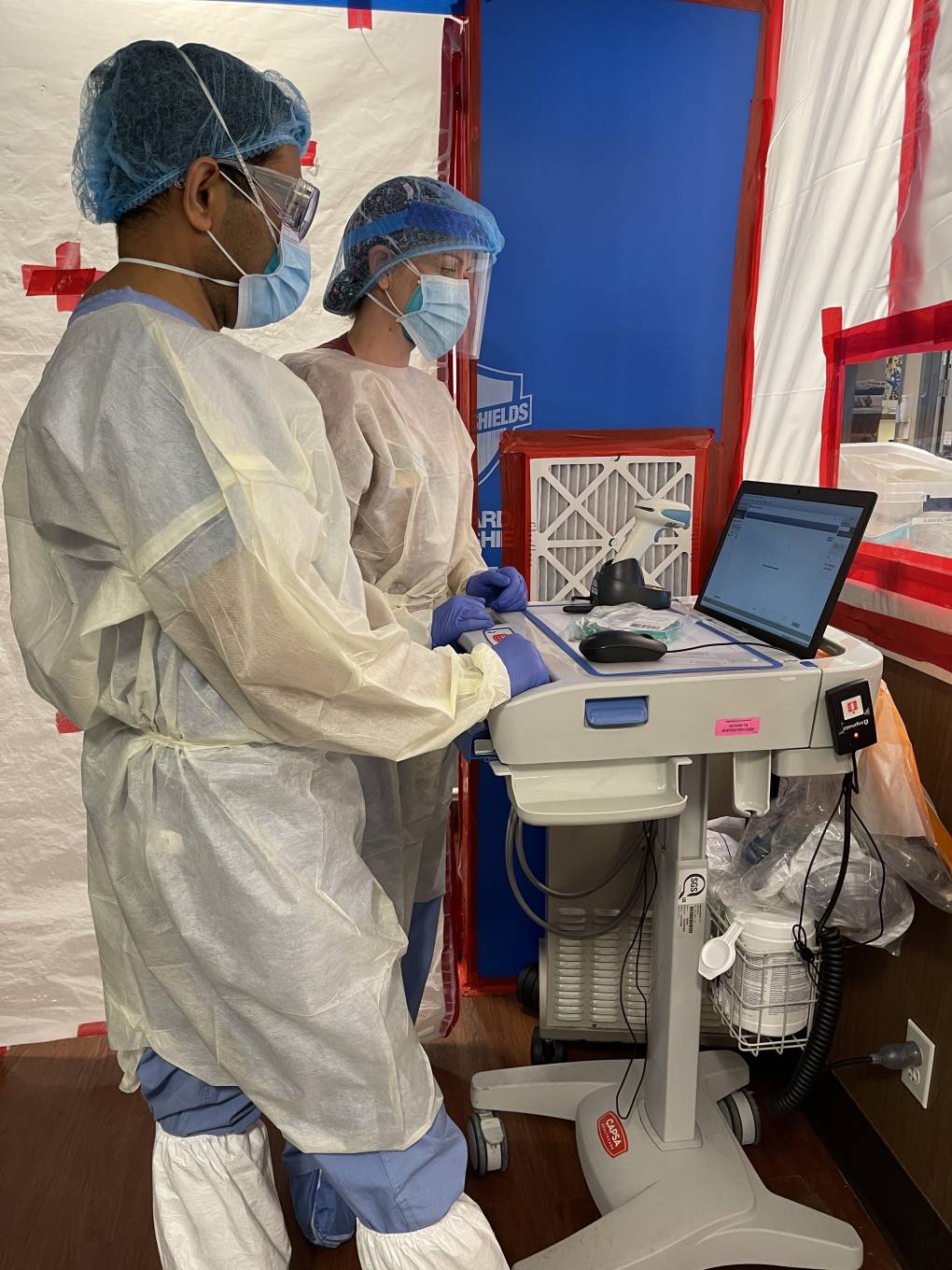
“The most important limiting factor is staff,” said Coyle. “Those critical care nurses, doctors and respiratory therapists that are needed at the bedside to care and to cure.”
The entire country is now suffering a shortage of health care workers with enough training to care for COVID-19 patients. Some who have those skills are at home taking care of children because schools are closed. Others are sick themselves or nursing loved ones. The virus has killed hundreds, potentially thousands of health care workers in the U.S.
Because hospitals across the country are running short on trained personnel, it’s making it harder for California to recruit from the same pool of overworked providers.
“We are mentally, emotionally and physically exhausted,” said Dinora Chinchilla, a pulmonologist specializing in critical care at a hospital in Orange County. “There’s only so many words you can use to describe the extreme fatigue.”
Watching the COVID-19 numbers soar is filling Chinchilla with dread. She says she can’t eat.
“Because this is real,” said Chinchilla. “I’ve had patients who’ve told me that they don’t believe that this exists until they’ve ended up in the hospital. Why have people lost faith in physicians? We practice this field because we love what we do. We want to save lives.”
She says it’s brutal taking care of so many patients who don’t make it.
“It’s like post-traumatic stress disorder that we all go through,” said Dr. Parimal Bharucha, a pulmonologist for Dignity Health in Sacramento. “It is a communal sense of grief. ”
He says his ICU is filled with motionless, sedated people kept alive by machines. The floor is strewn with masks and gowns. Nurses race between patients. It’s “like a war zone,” he said.
“Yesterday I was on-call for telemedicine and I had three patients crash within five minutes of each other,” Bharucha said. “At the same time, in another hospital, there were three patients who had cardiac arrest, one after another.”
Often, he can’t honor his patients’ dying requests. There was an older woman who hadn’t seen her estranged son in decades. She called him but he wasn’t allowed to visit his mother during her final moments because pandemic protocols prevent visitors from entering hospitals.
“This lady could not have the son at the bedside, and she treated me as a son and wanted me to hold her hands when she died,” said Bharucha. “And I could not live up to that.”
Just before she died, Bharucha was called away to treat someone else.
“Somewhere in the back of my mind, it is haunting me,” he said, tearing up.
Coyle attributes the current surge to increased virus transmission over Halloween. The sharp spike does not include the additional numbers doctors expect to see from Thanksgiving gatherings and travel.
So the situation is likely to get worse before it gets better. Dr. Bharucha’s hospital hasn’t had to turn anyone away yet, but he says that could change overnight.
“Please help us help you,” he pleaded. “Please help us take care of the people who really need our help. Don’t let hospitals be overwhelmed, because ultimately, at the end of the day, it is somebody’s loved ones who will need us.”
He urges everyone to stay home and sit tight over the holidays.