There is a weapon that is released by algae around the world and concentrated, invisible, in the flesh of shellfish. An amount the size of a poppy seed is enough to kill a grown person.
It’s part of an onslaught from which we’ve defended ourselves for decades, which might be why you’ve never heard of it.
Saxitoxin is lethal at concentrations 1,000 times lower than is cyanide. It is a powerful neurotoxin released by plankton in algal blooms. Saxitoxin is so potent, in fact, that it was the only marine toxin declared a chemical weapon by the 1993 international treaty known as the Chemical Weapons Convention, and bears a long and complex history with the U.S. government in particular.
The CIA reportedly gave pilots of U-2 reconnaissance planes a coin containing saxitoxin that they could use to commit suicide if they were captured. President Nixon ultimately banned the military’s use of biological weapons, including saxitoxin, in 1969, but the CIA neglected to destroy a stockpile of 10 grams of the substance that it had distilled from butter clams. The supply was rediscovered in a storage facility and distributed to scientists at NIH after a pharmacologist begged the CIA not to destroy the cache. He predicted, correctly, that the toxin’s potency offered enormous potential for medical research.

In both marine and freshwater systems, shellfish accumulate saxitoxin and concentrate it into doses dangerous to humans, fish, birds and marine mammals, although the shellfish themselves remain unharmed. The toxin is undetectable by sight or smell and is heat-stable, which means that even a pan-seared toxic mussel is still a toxic mussel.
When ingested by humans, saxitoxin causes paralytic shellfish poisoning, or PSP, symptoms of which include tingling, numbness, and, if consumed in high enough quantities, paralysis, asphyxiation and death. There is no known cure for saxitoxin poisoning.
California’s History of Toxin Monitoring
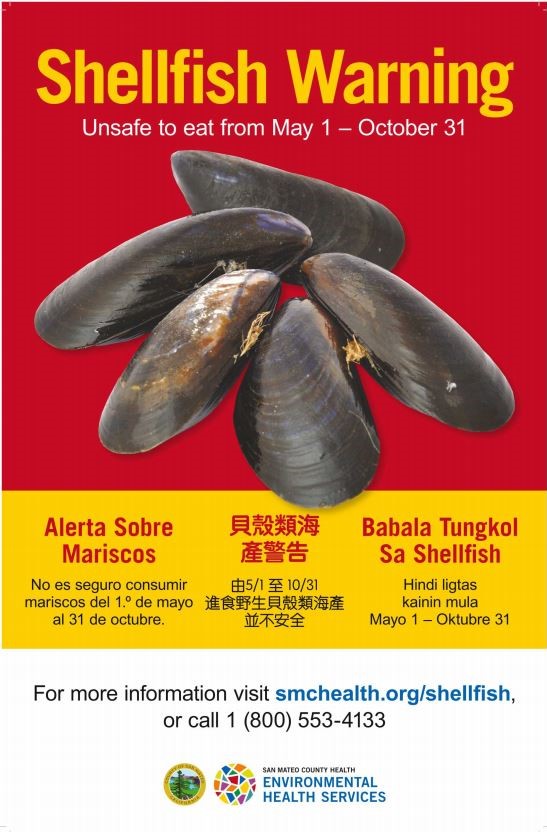
So why haven’t you heard of this potent algal toxin? Thank state health officials. In California, risk is managed by the diligent monitoring of the California Department of Public Health. Every year, CDPH issues a mussel quarantine for all coastal areas from Oregon to the Mexican border between May 1 and Oct. 31, adjusting its window according to changes in saxitoxin concentration. When concentrations are dangerously high, the state prohibits all recreational harvesting of mussels.
The public health department requires commercial seafood harvesters to submit shellfish samples at least weekly to retain their certification, which is one reason shellfish are available even when bans are in place. However, no commercial shellfish harvest occurs in San Francisco Bay, and that’s because, while coastal shellfish are monitored for paralytic shellfish toxins, no such monitoring occurs in the bay.
Some of the earliest recorded instances of saxitoxin poisoning occurred in San Francisco, before seasonal bans were commonplace, even before scientists knew what was poisoning their coast. In 1927, more than 100 people fell ill and six people died from paralytic shellfish poisoning. Panic spread. Public health workers quickly posted warning signs and scientists worked to identify the source of the widespread sickness. No cases were reported the following year, perhaps, as noted in a scientific paper published in 1937, because “people showed little desire, after the experience of 1927, to gather shell-fish.”
For the most part, the monitoring that began in 1927 has kept poisoning numbers low; Dr. Eddie Garcia, a fellow in medical toxicology at UCSF and the California Poison Control Center, says that in 2017, only 117 cases were reported across the entire United States, none of them fatal.
Why Saxitoxin is Relevant Now
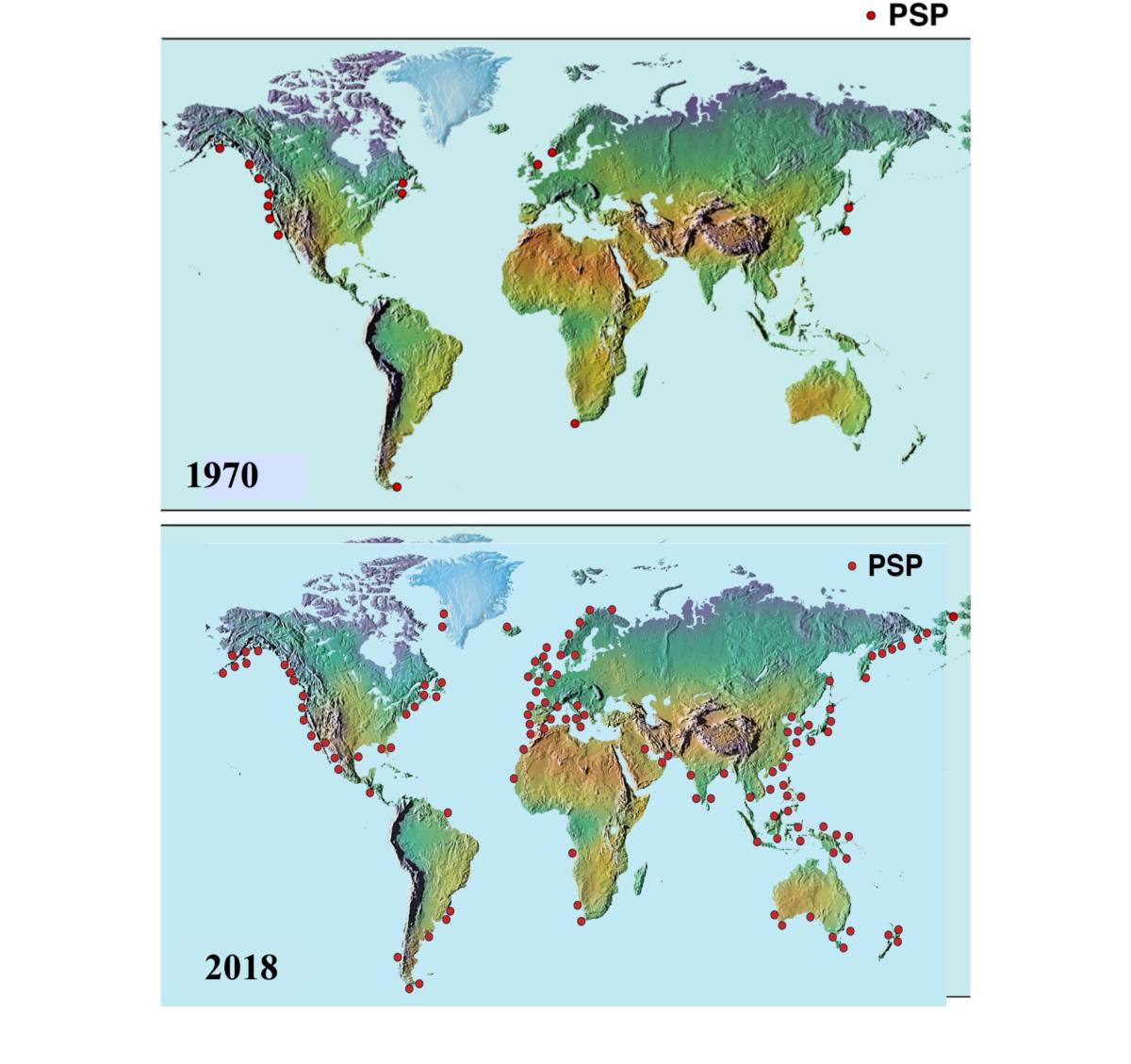
Scientists agree it’s critically important to have infallible toxin detection methods, particularly in the coming years. For one thing, experts say algal blooms are becoming more common, likely due to pollution and climate change, among other reasons. And even with decent monitoring already in place, some people are still getting sick.
“In a sense, it’s like a bad intersection where, if you put up some good traffic lights, you can improve it a lot,” said Don Anderson, a biologist at the Woods Hole Oceanographic Institute, who has spent more than 40 years studying harmful algal blooms. “It’s the people who don’t obey the restrictions, whether it be a stop light or a closure, that get sick.”
In 2014, for instance, a family vacationing on the coast of Washington made a soup out of mussels. It was midnight, too dark to read the signs that might have warned them not to eat shellfish they had caught themselves, and all seven ended up in the emergency room. One woman lost the ability to stand. The next day, the Washington Department of Health detected a saxitoxin concentration over 75 times the alert level.
Even in daylight, not every Californian might be aware of the quarantine; some may not be able to read signs because of a language barrier, or they may think different rules apply. If you’re relying on the old adage that you can’t eat mussels in months without the letter ‘r’, for example, it’s time to update your guidelines — this belief can be traced all the way back to at least 1599, when a cookbook warned against consuming oysters during summer months, most likely because bacteria were especially rampant during summer heat without refrigeration.
Although widely performed, saxitoxin testing is not terribly humane. In order to determine saxitoxin concentration, the most popular of three FDA-approved methods is to inject a mouse with a small amount of liquid containing an expected toxin, wait for the mouse to die, and record the time of its last breath. According to Maggie Broadwater, acting Harmful Algal Bloom Program Manager at NOAA, this mouse test is still used by CDPH to monitor toxin levels. Other methods do exist, but they involve transporting samples back to a laboratory and days of testing.
As algal blooms become more frequent and we begin to better understand how saxitoxin levels change, new methods have emerged that may transform the dynamics of our relationship with toxins — how we detect them, how we treat them, and how we learn from them.
A Lesson from the Bullfrog
The future of saxitoxin detection may come from an unlikely source: the common bullfrog. Researchers at UCSF published a recent study describing the structure of a protein called saxiphilin. It’s found in the heart and blood of the American bullfrog, which is resistant to saxitoxin poisoning. Using x-ray crystallography, researchers in the laboratory of Daniel Minor, professor at the Cardiovascular Research Institute, identified a pocket-like region in this protein that binds to saxitoxin. Scientists think that the bullfrog’s store of saxiphilin naturally reduces the concentration of saxitoxin in its bloodstream, giving the liver time to destroy the toxin.
Structurally, the protein and its binding pocket look a lot like transferrin — that’s a family of proteins that bind to iron and ferry it around the body. Saxiphilin is so similar, in fact, that Minor believes the two proteins must share a common origin.
“This is really evolution at work: repurposing a protein scaffold to do something else,” he said.
The ability to bind to saxitoxin could also someday lead to a treatment for shellfish poisoning. It might provide scientists with a blueprint for developing synthetic molecules that could be administered to patients who digest the toxin, to prevent paralysis.
A New Vision for Monitoring Shellfish
Scientists are also designing new-generation detection methods to improve coastal monitoring efforts. A hundred miles south of UCSF, scientists are developing a robotic technology that could replace the mouse-poison test. A team of researchers at the Monterey Bay Aquarium Research Institute has a device they affectionately call “lab in a trashcan,” or more officially, Environmental Sample Processor.

