He said the preliminary research shows that this virus may spread more easily among humans than SARS or MERS, but it appears to be less lethal. Researchers estimate the mortality rate of COVID-19 at about 2 percent, compared with about 9 percent for SARS and more than 30 percent for MERS.
Greene added that it’s still too early to know this for sure because the data are “rapidly evolving.”
“My message,” he said, “is that this is an outbreak. It’s not an epidemic.”
He and other panelists said influenza poses a greater threat to public health compared to this novel coronavirus.
“In general, around 35,000 people die every year of the seasonal flu,” Greene said.
So far this flu season, the federal Centers for Disease Control and Prevention estimates that more than 20 million people in the United States have contracted influenza, and more than 10,000 have died.
Only 15 people in the U.S. have so far tested positive for COVID-19.
Tracking the Virus
Researchers have traced COVID-19, and viruses like it, to bats. Animal-to-human transmission, however, typically occurs through a secondary host. Scientists have traced the MERS outbreak to palm civets (a cat-like mammal), and SARS to camels.
Greene said public health experts don’t yet know the secondary host for this strain of coronavirus, but they believe the outbreak began at a seafood market.
Dr. Charles Chiu, director of the UCSF-Abbott Viral Diagnostics and Discovery Center, said the initial animal-to-human transmission likely occurred in late November or early December of 2019.
“Since then, there’s been no evidence of ongoing animal-to-human transmission events. All of the outbreak has essentially been sustained by human to human transmission,” Chiu said.
Panelists said a shortage of samples has limited their research. Chiu said scientists do have access to at least 60 genome sequences of the strain from different patients. From these sequences, scientists have discovered only seven mutations.
“The virus, in general, is not regarded as a very fast mutating virus. This is unlike other viruses that we have that can adapt very fast,” said Dr. Melanie Ott, a senior investigator with the Gladstone Institutes.
That may be a boon to researchers working on vaccines and treatments.
Containing the Outbreak
At present there is no cure or vaccine specific to COVID-19.
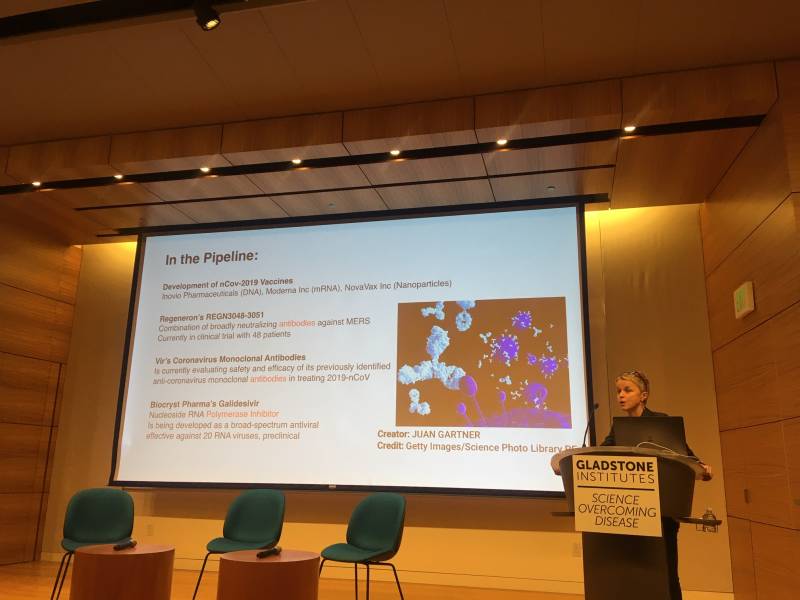
Ott said at least three companies have publicly announced the development of a vaccine.
“Interest in making a vaccine is very high currently,” she said, “… either with a DNA and RNA, or with a nanoparticle vaccine.”
Ott added that physicians are in the process of testing antiviral drugs for the flu, HIV, MERS and ebola in patients with COVID-19.
Researchers with the National Institutes of Health’s National Institute of Allergy and Infectious Diseases say vaccine candidates could be available for human testing in about three months. But it will likely take about a year to complete validation and safety evaluations.
Greene said public health measures hold the key to containing the outbreak.
“SARS was not controlled by medicines or a vaccine. It was controlled by public health interventions, tracking infections, limiting contact of infected individuals with others. And certainly in the absence of appropriate vaccines and and highly active drugs, that’s exactly what will be undertaken here,” Greene said.
He added that a strain on resources is the big challenge for health officials in China.
“We now see or are hearing reports that in Wuhan that there are sick individuals who are wandering from hospital to hospital trying to get care. They’re running out of supplies. The medical system is completely stressed,” Greene said.
But unlike the the more pervasive flu, he said, this novel coronavirus doesn’t have “the same type of seasonality,” meaning, once contained, it likely won’t resurface each year.
Masks Not Generally Recommended
The CDC doesn’t recommend masks for most people.
“Medical personnel in close contact caring for patients with chronic viruses should take all precautions. But in terms of day-to-day interactions, hand-washing is far more effective,” Greene said.
The CDC does recommend masks for patients with the virus, people in their households and hospital staff treating them.
“The final message I think we want,” Greene said, “is we should be watchful…we should follow this outbreak, but we should be secure in the fact that the apocalypse is not upon us. This is a viral outbreak that is running its course now.”