Lee stressed that most people could reduce their own individual increase by shopping around.
"Almost 80 percent of our customers could either pay less than they are paying today or pay no more than [a] 5 percent increase," Lee said, if they comparison shop.
Larry Levitt, senior vice president at the nonpartisan Kaiser Family Foundation, agreed there may be "deals to be had."
“The market is still working much better in California than in most other states," he said. "It’s quite competitive in giving consumers a large number of choices."
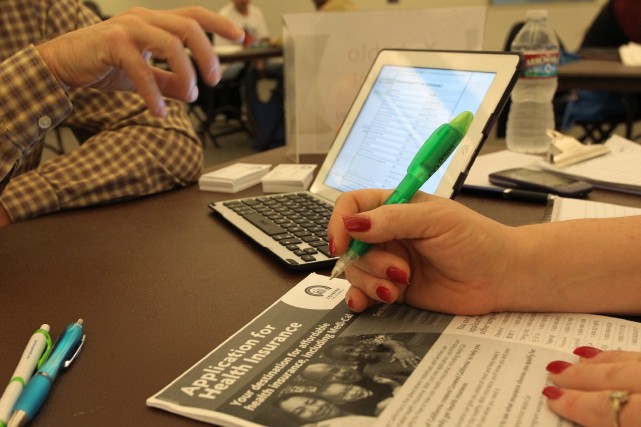
About 1.4 million Californians purchase their health insurance through the Covered California exchange.
Blue Shield and Anthem Blue Cross customers will face the steepest increases. They have about "a quarter of the market each," Lee said. Anthem customers will see a statewide average increase of 16 percent, and Blue Shield is "above 19 percent," Lee said.
In the Bay Area, those increases will be even steeper for Anthem and Blue Shield customers. Meanwhile, the average monthly premium hike for Kaiser members will be in the 5-6 percent range across much of the region.
"We are committed to offering stable rates over the long term," said Bill Wehrle, a vice president at Kaiser Permanente, "and are uniquely positioned to deliver more affordable health care coverage." He cited investments in technology and Kaiser's "emphasis on wellness" as factors keeping premium increases lower.
Here are some of the proposed rate increases for major plans in several Bay Area counties:
San Francisco
Average increase: 14.8 percent
Kaiser: 5.3 percent
Anthem Blue Cross: 16.7 percent
Blue Shield: 24.2 percent
Contra Costa County
Average increase: 13.6 percent
Kaiser: 5.6 percent
Anthem Blue Cross: 22.6 percent
Blue Shield: 24.4 percent
Alameda County
Average increase: 12.3 percent
Kaiser: 5.6 percent
Anthem Blue Cross: 23.7 percent
Blue Shield: 18.9 percent
Santa Clara
Average increase: 9.2 percent
Kaiser: 5.6 percent
Anthem Blue Cross (EPO): 8.4 percent
Blue Shield: 22.3 percent
You can look up the proposed rate for your plan in your specific area by checking Covered California's rate booklet.
The rates are not yet final. State regulators will review them in the coming weeks.
Original post:
California's Obamacare customers can expect a hefty increase in their monthly health insurance premiums next year. Covered California will announce new 2017 rates Tuesday morning for people who buy their plan through the state marketplace, and experts are predicting that increases will be double or even triple what they were last year.
“2017 is going to be a transition year,” said Peter Lee, executive director of Covered California, testifying before Congress last week. “We expect our rates to be higher than we saw in our first two years.”
In 2015 and 2016, marketplace premiums increased an average of 4 percent -- a rate celebrated by consumer advocates as “modest,” even “terrific.”
Covered California’s proposed budget for 2017, released in May, projected average rate increases of 8 percent. Industry insiders are suggesting the average jump could be even higher.
There are three key reasons why.
One: Medical Costs are Up
Insurance companies say premium prices are going up because medical costs are going up. Doctors, hospitals, labs and pharmaceutical companies are all raising their prices.
“Unquestionably, runaway drug prices remain a serious problem,” said Charles Bacchi, president and CEO of the California Association of Health Plans, a trade group for insurers. “We’re seeing new drugs coming out with blockbuster prices, and we’ve seen drugs that have been around for 30 years double and triple in price for no reason.”
Northern Californians have felt the burden of higher medical costs more so than people in Southern California because the hospital market is more consolidated, giving hospitals more bargaining power with insurers.
Early rate filings from other states indicate rising medical costs could contribute to premium increases anywhere from 3 to 9 percent.
California regulators will have a chance to review the proposed rate increases, and consumer advocacy groups say they look forward to participating in the process by challenging some of the assumptions health plans have made about costs.
"To the extent insurers are booking a certain amount of medical inflation to prescription drugs, are they overestimating those costs?" said Anthony Wright, executive director of Health Access. "Is that a scapegoat or a true driver?*
Two: Federal Protections are Expiring
The Affordable Care Act established a “reinsurance” program that was designed to help insurance companies cover losses if they had a high proportion of really sick, expensive patients. Insurers didn’t know who was going to sign up for their plans, and basically had to guess how sick they would be and how much care they would need, then factor that into their premium rates.
Through the reinsurance program, all health plans paid into a shared pool, then those funds were distributed to companies that ended up with more high-cost patients. This meant plans didn’t have to make up losses by increasing premiums the following year. But that protection expires this year, adding a 4 to 7 percent increase to consumers’ monthly premiums in 2017, according to an analysis of the American Academy of Actuaries.
Another program, "risk corridors," which is designed to protect consumers against excessive premium increases, also expires this year.
Three: People May Be Gaming the System
Most people buy their insurance during the set enrollment period starting in the fall. But people who lose their coverage during the year because they lose a job, get divorced or move (among other eligibility criteria) are able to buy a plan through Covered California outside normal enrollment periods.
But insurers are noticing that these customers have medical costs that are 25 to 40 percent higher than the rest of the health care population, said Bacchi.
Are people taking advantage of the system, signing up for coverage not because they had a qualifying change in life circumstances, but because they got sick? Or is it that sicker people are more motivated to look for ways to stay insured after they lose coverage through work or a divorce?
Californians May Be Better Off
Despite all these factors, state officials and the insurance industry say Californians are still better off than consumers in most other states. Peter Lee emphasized that Covered California is an “active purchaser,” meaning it negotiates with plans when they set their prices.
“Covered California does not negotiate by table-pounding, but rather by providing good data on the risk mix of who is enrolled and working the health plans to garner maximum enrollment,” Lee said in his remarks before Congress. “In 2015, we provided data that proved Covered California enrollees were healthier and presented less risk to insurance companies than anticipated, which helped drive down the cost of health premiums.”
Bacchi said consumers here also have more choice.
“We have a highly competitive health care market, with 11 health plans in Covered California duking it out over price and quality and in most of the regions of the state,” said Bacchi.
Health advocates say consumers should take advantage of that by shopping around for a better deal. So even if the average premium increases 8 to 12 percent, that doesn't mean every single plan jumped that much.