Staff say the tests are in such short supply that symptomatic patients may be slipping through the cracks. As for employees who’ve shown symptoms, many have not been able to get tested in the community.
“You send me home. I call my doctor. They say self-quarantine,” Garcia said. “But I don’t know if I’ve actually had it or not, and if I am positive, I’ve exposed people at work. But we’ll never know who.”
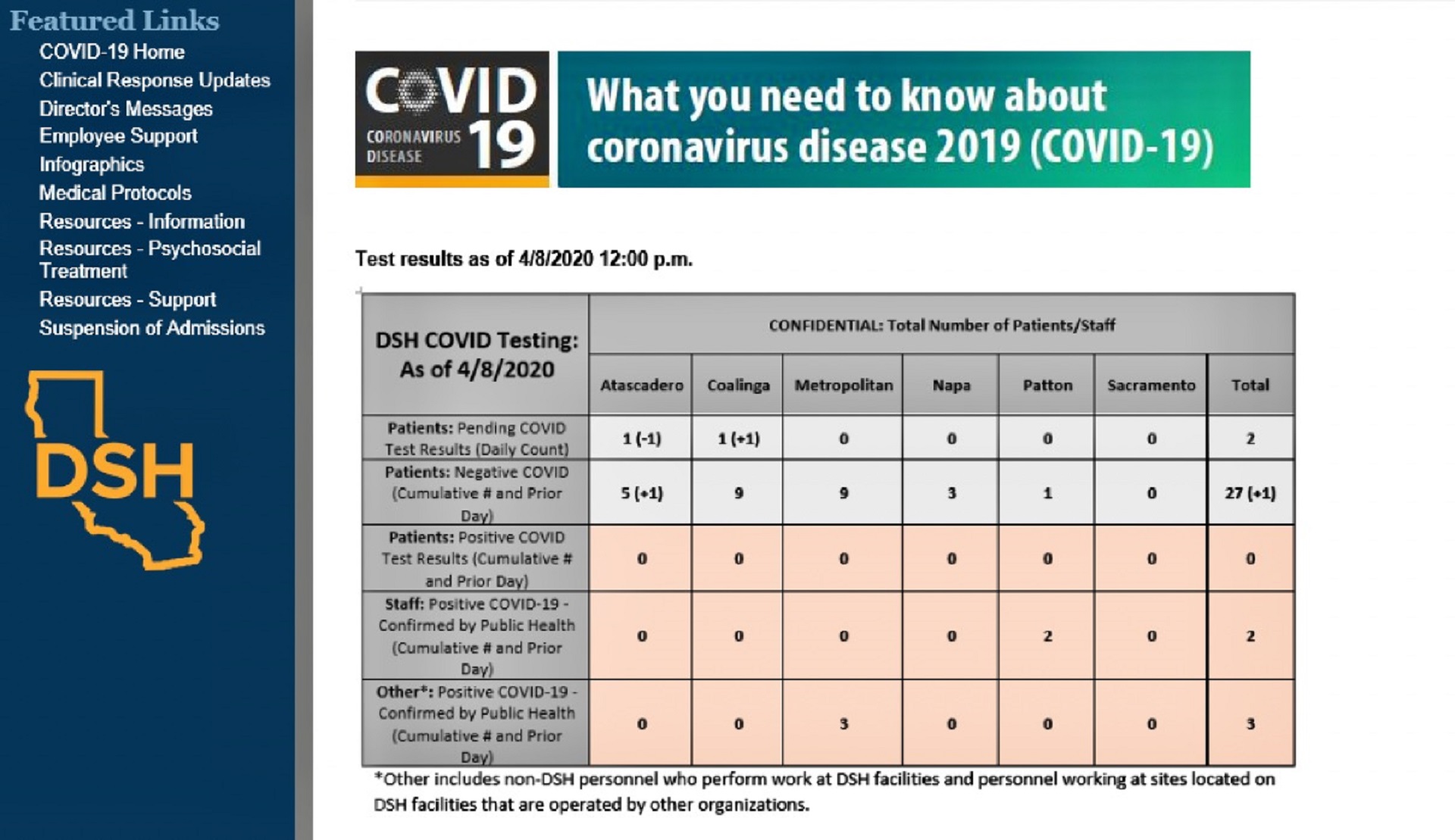
While jails and prisons can confine inmates to their cells to avoid the spread of infection, the state hospitals — which also include Napa State Hospital, Coalinga State Hospital and Atascadero State Hospital on the Central Coast — cannot.
The vast majority of men and women confined in the state hospital system have been accused or convicted of crimes directly linked to their mental illness. Yet the hospitals are treatment facilities — not prisons — and patients move about freely in their units. Many employees, including psychiatric technicians, registered nurses, rehabilitation therapists and psychologists, interact closely with them daily.
Still, not all staff are taking precautions.
The hospitals only recently began issuing one surgical mask per day to all employees. Those can prevent the spread of contamination by the wearer. The N95 masks, which protect the wearer against outside infection, have been doled out more selectively to staff “working in higher risk situations” with patients known or suspected to be carrying the virus, state officials said.
Yet, according to interviews and internal emails shared by staff, wearing a surgical mask remains voluntary, except at Patton, where administrators last Thursday informed employees that a San Bernardino County public health order now requires it.
One clinician, who asked not to be named because management instructs employees not to speak to reporters, said that there were “a significant number of people who work at Patton who are not wearing masks, not wearing gloves, not practicing social distancing. People are sharing pens. You have people who are taking this extremely seriously working next to people who aren’t.”
That could prove tragic, as many patients are elderly and others have underlying health conditions due to medication side effects and poor self-care, among them obesity, diabetes and hepatitis C.
Jaime Garcia, who works at Coalinga State Hospital and is that facility’s president of the California Association of Psychiatric Technicians, said the workers he represents “are basically making a choice on whether they wear a mask or not.”