Skip to:
- Sex and Physical Contact Risks
- Dating During a Pandemic
- Temporary Alternatives for Sex and Dating
- Advice for Cohabiting Couples
Note: This guide to sex and dating includes some graphic language.
Let’s get this straight: during the COVID-19 pandemic, there is no “safe way” to have sex with someone you don’t live and quarantine with.
But humans are humans, and we know some folks will still make the choice to get physically intimate with other people, despite the presence of a highly contagious disease in our midst. So we asked for your anonymous questions, and created this guide to sex and dating during the coronavirus pandemic.
Because there’s no 100%-safe way to date or have sex outside your household right now, you’ll see the super-unsexy — yet super-important — phrase “harm reduction strategies” throughout this guide. That’s because when it comes to engaging in social and physical intimacy, it’s all about weighing your risk factors, assessing them against the risk factors of the person (or people) you’d like to have sex with and doing everything you can to further reduce the potential harm.
We’ve consulted with these sex and health experts:
- Stephanie Cohen, medical director of San Francisco City Clinic
- Nenna Joiner, owner of Oakland sex store Feelmore and former adult filmmaker
- Julia Feldman, Bay Area sex educator and consultant at Giving the Talk
Sex, Physical Contact and COVID-19

What bodily fluids can carry COVID-19?
So many aspects of the coronavirus remain mysterious to scientists, and that includes the full scope of COVID-19’s relationship with sex. But here’s what we do know.
If someone has COVID-19, they can transmit the virus via particles in:
- Their saliva
- Their mucus
- Their breath
The coronavirus has also been found in the semen and feces of people with COVID-19. It hasn’t been found in vaginal fluid.
Can COVID-19 be spread through sex, whether vaginal or anal? The scientific community actually doesn’t know for sure yet. What we do know is that “sex is the definition of close contact,” as Stephanie Cohen puts it. So if you’re close enough to get physically intimate with someone with COVID-19, you’re definitely close enough to have a high risk of being infected via those particles they’re exhaling.
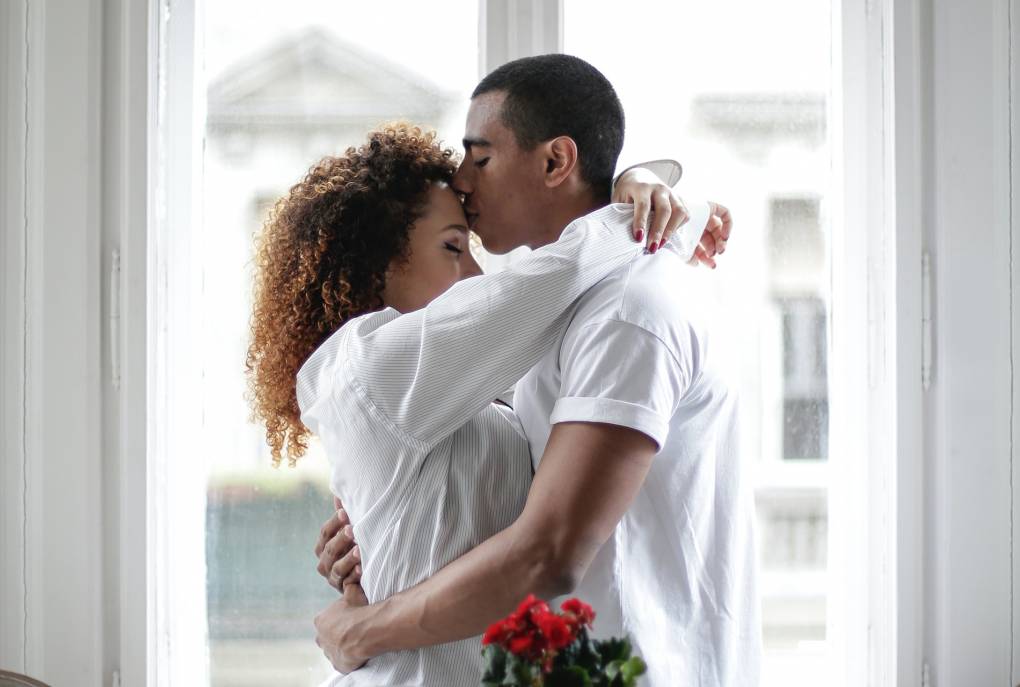
How dangerous is kissing?
Kissing someone outside of your household is one of the most risky things you can do right now, Cohen says, because of how much exchange of saliva it involves.
For this reason, she says, kissing might actually present a higher risk of transmission than vaginal or anal sex. And anything that increases your respiration and your respiratory rate “will likely result in the release of more respiratory droplets,” thus increasing the risk of transmission — think heavy breathing.
Are certain types of sex riskier?
Because the coronavirus has been found in feces — and because gastrointestinal symptoms like diarrhea can occur sometimes with COVID-19 infection — Cohen says there’s a likely chance that anal sex or oral-anal contact would pose more of a transmission risk than other forms of sex such as penile-vaginal contact, for example.
That said, medical professionals just don’t know for sure. COVID-19 transmission risk would also be impacted by a number of other factors, such as the degree of face-to-face contact and how infectious the person with COVID-19 is at the time of the sexual encounter. Right now, there just isn’t enough data to be definitive, Cohen says — so it’s all about assessing those various risk indicators we do know about.
If I do have sex, what are some things I can do to reduce my risk of catching COVID-19?
If you’re utterly determined to have sex outside of your household right now, these precautions represent harm reduction strategies:
- Wearing a mask: Remember, a mask protects the other person in how it limits the spread of your respiratory droplets. For masks to truly reduce the risks of either sexual partner getting COVID-19, both people would have to wear a mask: a mutual masking, if you will. “It might not be a strategy that works for everyone,” Cohen says, “but certainly I think it’s one that could reduce risk.” Remember though: as Nenna Joiner reminds us, masks are like condoms in the sense that you “still need to know how to put [them] on correctly.”
- Choosing positions that minimize face-to-face contact: Spooning sex, doggy-style, reverse-cowboy/cowgirl/cowperson — consider agreeing to stick to sexual arrangements that keep your faces far apart, and ideally with one person faced completely away from the other. (It’s a bit of a spontaneity-killer, yes, but it’s a good idea to agree to this one before you start having sex, to avoid ‘the heat of the moment’ making the decisions for you.)
- Remember cleanliness: “Washing up really well, both before and after sex” is another way sexual partners can potentially reduce their risk to each other, Cohen says. Wash your hands often with soap and water for at least 20 seconds. If you don’t have soap and water on hand, use a hand sanitizer that contains at least 60% alcohol and rub your hands together until they feel dry. Don’t use sanitizer anywhere intimate — it will really irritate that delicate skin. If you have someone else’s bodily fluids on your body, be sure to wash them off thoroughly. You cannot “absorb” the coronavirus through your skin, but you might touch your skin and then touch your face. If you’re using sex toys, wash those with soap and warm water.
- Using condoms and other barriers: Wearing a condom during sex will decrease your exposure to saliva or feces. For oral sex, using a condom or dental dam similarly provides a barrier. This is especially important for any anal contact.
- Keep it quick: Minimizing the length of a sexual encounter is a harm reduction strategy in how it’s reducing the amount of time you’re potentially being exposed to the virus.
- Consider things that don’t exchange fluids: Mutual masturbation could be considered a harm reduction strategy, Cohen says. But don’t forget that if you’re simultaneously making out, “that could actually be higher risk than a quick session of oral sex,” she says.
And remember: Don’t forget to practice the safe sex you usually would before the pandemic.
With all this in mind, we’ll say it again: right now, during the COVID-19 pandemic, there is no way of having sex with someone outside your household that carries zero risk of transmitting or obtaining the virus.
“Everyone’s looking for a magic loophole,” acknowledges Julia Feldman, “and it doesn’t really exist.”
And here’s another tricky thing. Even if you and your partner agree to abide by all of the above harm reduction strategies in the cold light of day, things can shift in the heat of the moment. Previously agreed-upon plans can fall apart when inhibitions are lowered and you’re turned on, especially if alcohol is involved — and in these circumstances “you’re less likely to use your prefrontal cortex to really analyze the risk involved in the situation,” Feldman stresses. “Especially if you haven’t had sex in a long time and you’re very excited to do it.”
So if you’re concerned that your safety boundaries might be in any way reduced or made negotiable during sex… back away, and prioritize your health.

OK… I had sex anyway. How long should I wait to get a COVID-19 test?
If you aren’t sure whether your sexual partner had COVID-19, the best time to get tested for the coronavirus would be between five and 14 days after the encounter, says Stephanie Cohen.
That’s because the median average time from exposure to coronavirus symptom onset is five days — so testing any earlier than that might not yield an accurate result — but the incubation period (the amount of time you can be infected before showing symptoms) is up to 14 days.
Is isolating for 14 days between sexual partners a good idea?
Here’s the idea: you have sex with someone, and then wait for 14 days to see if you develop symptoms of COVID-19. If you don’t, you’re good to move on to a new partner safe in the knowledge you don’t have the disease and aren’t passing it on — right?
Not quite.
“It’s a good strategy; it’s a harm reduction strategy,” Cohen says, but “it’s not a zero-risk strategy.” That’s because of the large numbers of people who get COVID-19 but never show any symptoms.
What about sex with more than one person?
Having multiple people that you have sex with is a definite risk factor for transmitting COVID-19. These kinds of overlapping sexual relationships with different people — going back and forth between people, basically — is called “concurrency” in the sexual health world, and it’s something experts say will heighten your risk of spreading the disease.
“To minimize that concurrency,” Cohen says, “decrease the network size — which decreases the spread of coronavirus.” Basically, consider reducing the number of people you’re having sex with during the pandemic.
Where does that leave you if you practice polyamory, which is all about having multiple sexual relationships?
Nenna Joiner says that yes, some folks are deciding to take a break from polyamorous intimacy during the pandemic owing to the heightened risks of having different partners right now. But other poly people are choosing to isolate together “as a poly family,” they say, and agreeing to only have sex “within that sphere of people.” Ultimately, it’s about finding the solution that works best for your health, and that of others.
What about group sex?
If group sex (having sex with multiple people at the same time) was your thing before the pandemic, Stephanie Cohen has a message for you: “The fewer people, the better.”
That’s because with every additional person in a situation — social or sexual — you’re adding a potential COVID-19 case, whether they know they have it or not. In a group sex situation, that person is then potentially transmitting the coronavirus to multiple people at one time — who could then go on to infect others, who then go on to… you get the picture.
If you do continue to choose group sex, New York City’s public health department advises you to “Go with a consistent sex partner” in such a situation, and “pick larger, more open, and well-ventilated spaces.”
What about sex workers? How can they make it work right now?
Is there a way to safely engage in sex work in the midst of a pandemic?
It’s “a profession that certainly carries risk,” Cohen stresses, due to the amount of close physical contact involved. In addition to the other strategies discussed here, some additional harm reduction strategies sex workers might consider are to limit the number of clients they see during the pandemic, to opt for a smaller circle of regular clients and “more spacing out in-between partners.”