Connection Is Key
Evans’ story is not uncommon. At the Curry Senior Center, where she lives, older adults who connect virtually with friends and family are doing well, says Angela Di Martino, the facility’s wellness program manager.
Technology, though, is not a panacea.
“Video calls cannot replace personal contact,” she said.
Di Martino is among the experts who fear virtual interaction won’t offer a meaningful substitute for live conversation in the long run. Zoom fatigue is a real thing.
Unsurprisingly, those seniors who are still engaging with people in person are faring the best. UCSF geriatrician Louise Aronson says she’s been hearing from older people who actually feel less isolated now than prior to the pandemic, because they live in multigenerational households, with family members who no longer rush off to work or school. Some are finding new purpose by helping their grandkids with distance learning.
1 in 4 Lonely
To be sure, not all seniors are riding out the storm smoothly. About 1 in 4 older adults say they’re anxious or depressed, according to a Kaiser Family Foundation poll, a rate that has more than doubled during the pandemic.
The isolation is especially acute in nursing homes that prohibit visitors. Aronson says she’s seen patients who are refusing to eat, or who cry alone in their rooms for long stretches. One recent study of 111 residents in a Chicago-area nursing home found the group had shed an average of about four-and-a-half pounds from December through April. The researchers attribute the changes to fewer social interactions, a halt to family visits, and shifts in schedule, driven by the pandemic.
“Because they haven’t touched another human being or been touched by another human being since March,” said Aronson, “there is isolation. There is depression. There is battle fatigue.”
Aronson points to a former patient of hers, Shirley Drexler, who died at an assisted living facility in San Francisco two months into the coronavirus outbreak. Though 102 years old, prior to the pandemic she was highly social, bright-eyed and steady on her feet. She used to dash from table to table to share lewd jokes during group meals, Aronson said.
“But after a few weeks, when it became clear that the coronavirus wasn’t going to go away, she basically took to bed and died. Because at 102, she wasn’t going to live long enough to see the end of it. And so she figured that was it.
“We’ve heard many other stories like that.”
A growing body of literature shows persistent loneliness has a number of consequences, such as depression, physical pain, increased disabilities and even death. Some research has shown a link between loneliness and the development of dementia, heart disease and stroke. A recent study for the first time showed an association between loneliness and diabetes risk.
One Day at a Time
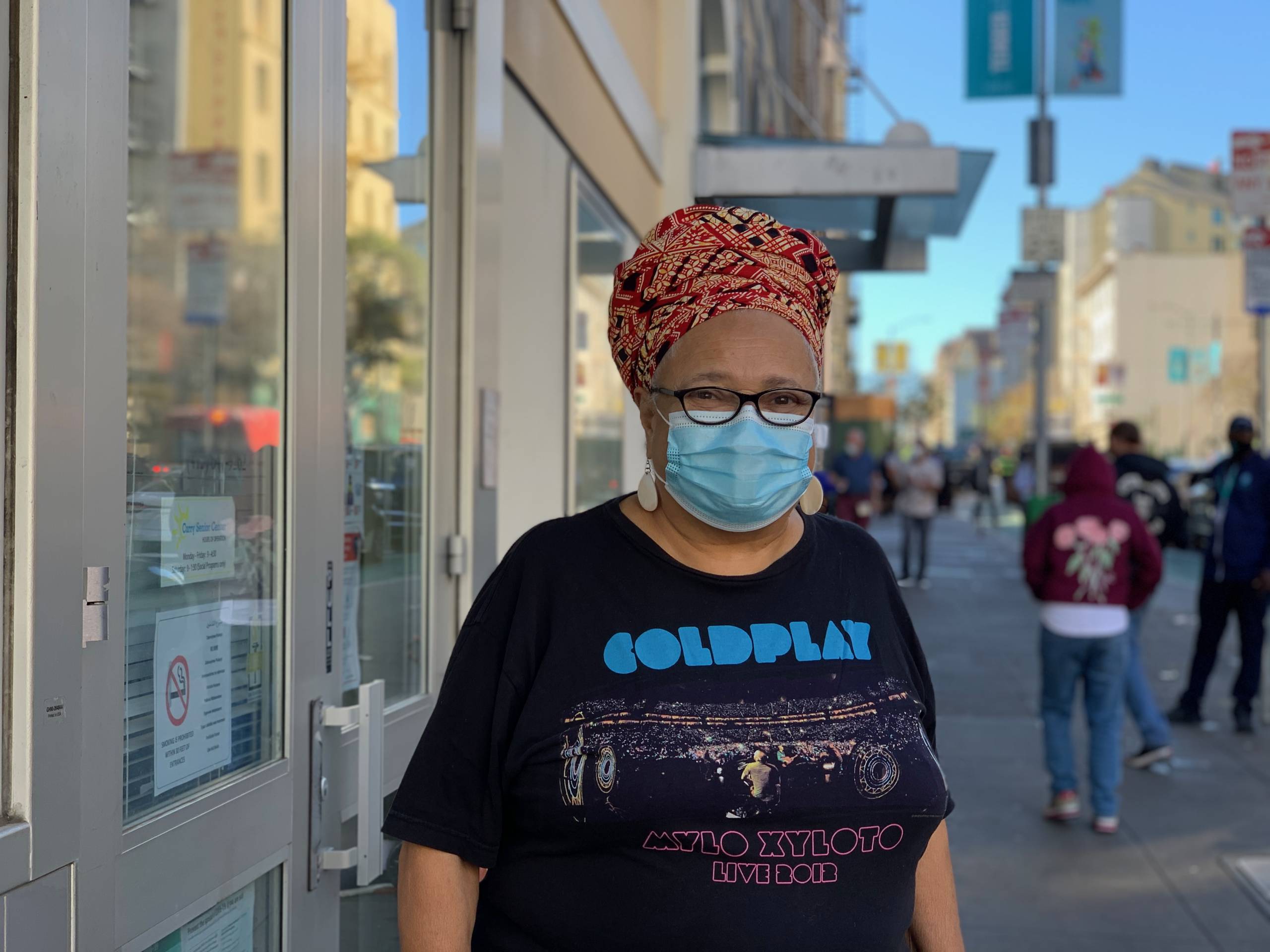
Sukari Addison is one of the lucky ones. Dressed in a stylish pair of silver earrings and gold glasses, she says her motto is not to worry about things she can’t control.
“We are in a really big change now,” Addison said. “But I’ve been through changes before. A lot of them as an African American.”
She suffers from congestive heart failure and high blood pressure, both of which are risk factors for COVID-19. But Addison is not living in fear.
“You get to be 85 years old, you know you got a foot on the banana peel,” she said.
On a hot summer night in August, after collapsing on her bed from fatigue, she tried not to panic. Within days she tested positive for COVID-19 and landed in the hospital with pneumonia. The hardest part, she says, was the no-visitor policy. After two dire weeks, her physician sent her home, and she credits her recovery to the kindness of the nurses and doctors.
She’s still moving slowly and spends most days alone in the room she rents near Union Square. But she says she’s not lonely, as her devices keep her connected.
“I learn so much because of technology,” she said. “All I have to do is turn on my iPhone or my iPad or my computer. And there is a new subject for me to learn.”
She often showcases her new skills over FaceTime with her six great-grandchildren on the East Coast. In the evenings, her sweetheart visits. They make dinner in her instant pot.
On difficult days she pulls on her gloves, tightens her mask and strolls the city, chatting with folks on the street. She looks forward to a lot more social interaction when the pandemic ends.
“I’m a professional volunteer!” proclaimed Addison. Until that’s safe, she’s taking it one day at a time.
“The good news overall is that older adults are adapting. They’re resilient,” Kotwal said. “They’re finding ways to continue to cope despite these really prolonged restrictions. On the other hand, I think there is that subgroup that has had persistent loneliness that hasn’t been able to adopt new technologies or has had trouble coping.”
Kotwal says it’s critical that doctors and social service agencies track older adults who may not have access to or feel comfortable navigating technology. He and his UCSF colleagues plan to check back with their original study cohort in a few months. He worries colder weather and a very different holiday season may lead to increased loneliness, and he suggests calling seniors more often this fall and winter.