Note: Pfizer COVID vaccine booster shots are now available for certain eligible groups. Find out who can get a Pfizer booster shot, and how to make an appointment near you.
You're not imagining it.
Back in mid-August, U.S. health officials announced plans to offer COVID-19 booster shots to all Americans, starting as early as this week (Sept. 20).
That hasn't happened.
And while the Food and Drug Administration has now authorized a booster dose of the Pfizer-BioNTech coronavirus vaccine for people age 65 and older and certain other groups, with endorsement from the CDC, you could be forgiven for wondering: What happened to this previous timeline? When could we actually see booster shots roll out? And who might get them first?
I thought booster shots for all were starting Sept. 20? What changed?
The original White House booster plan for the general public, announced on Aug. 18, called for an extra dose eight months after getting the second shot of the Pfizer or Moderna vaccines. (That time frame was since revised to six months.) The one-shot Johnson & Johnson vaccine was not included in the plan.
But in the last several weeks since the Biden administration's announcement, a lot has changed. According to The New York Times, the projected September time frame "set off alarm bells" among officials in the FDA.
Earlier this month, top federal health officials allegedly warned the White House that it should scale back its booster-shot plan, the NY Times reported. Representatives from the FDA and the Centers for Disease Control and Prevention purportedly told the Biden administration they would need more time to review all the available data.
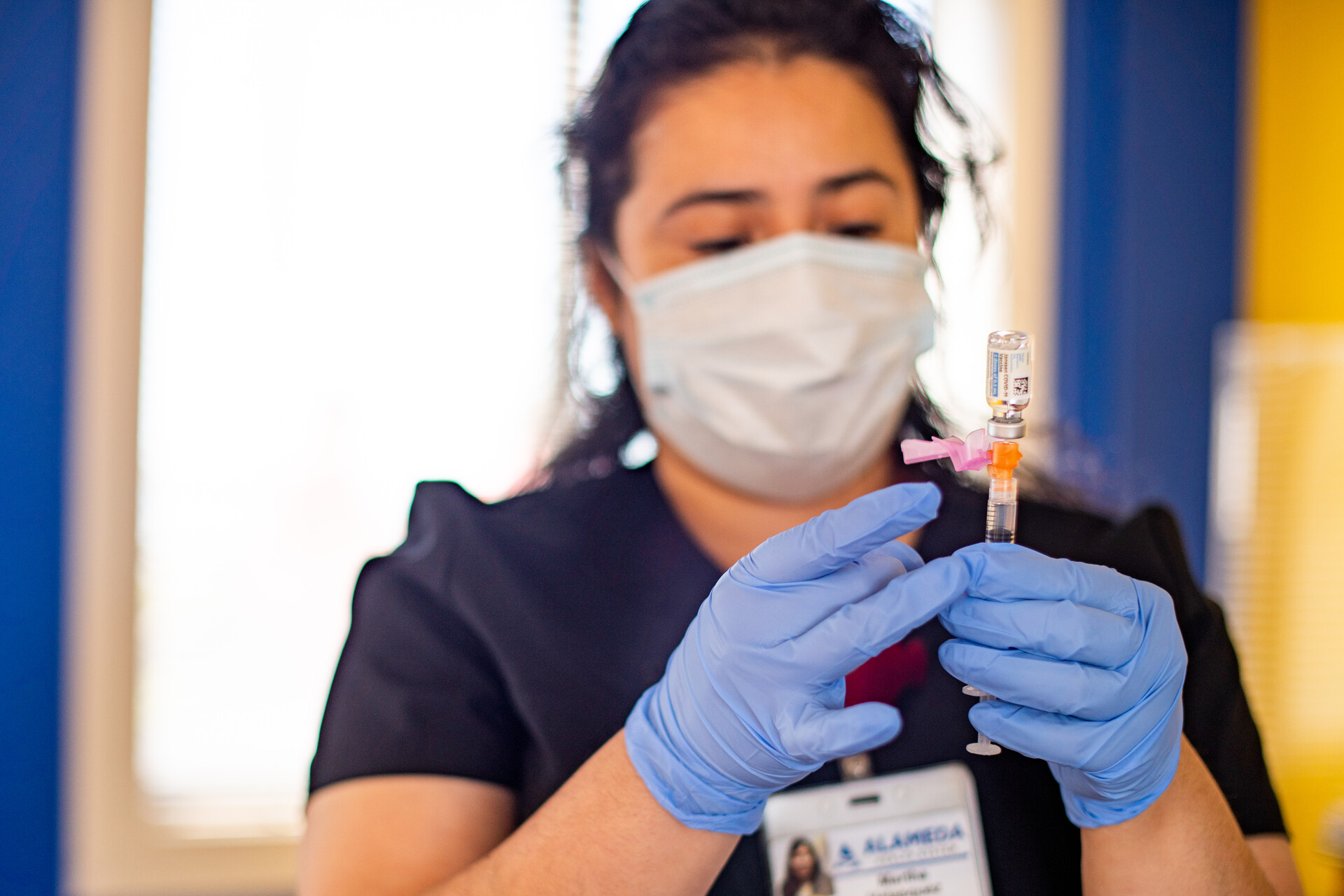
COVID-19 vaccine manufacturers have been conducting their own research into the efficacy of booster shots for their particular vaccines. The next stage on the road to booster-shot approval for any particular manufacturer is a review by an advisory panel of experts convened by the FDA. This panel is a part of the FDA's overall evaluation of the safety and effectiveness of a third dose, which is also being reviewed by a CDC advisory panel.

But now we have one approved vaccine booster, right?
Yes. On Sept. 22, the FDA authorized a booster dose of the Pfizer COVID-19 vaccine. But this booster shot only applies to people who have gotten the Pfizer vaccine for their first two shots, and who:
- Are 65 and older
- Are at high risk of experiencing severe COVID-19 symptoms
- Have jobs or institutional exposure to the virus that puts them at high risk of contracting COVID-19
The FDA says that a third shot can be given at least six months after completion of a person's last Pfizer shot. On Sept. 24, the CDC formally signed off on the plan.
This means these eligible groups will be able to get their Pfizer booster shot in California soon. The Western States Scientific Safety Review Workgroup — which represents California, Nevada, Washington and Oregon — will now independently review the FDA and CDC recommendations, and only then can any of the coronavirus vaccine boosters be distributed in California.
This FDA authorization comes after the organization's advisory panel met Sept. 17 and voted 16-2 against a plan to use Pfizer boosters for people 16 and older. The same experts did, however, vote 18-0 in support of the FDA authorizing a booster for people 65 and older or at high risk of severe COVID-19. The FDA typically follows the advice of its advisory committees — although they're not required to.
On Sept. 23, the CDC's own advisory panel met to make specific recommendations about use of this Pfizer booster. The CDC panel aligned with the FDA authorization in all respects, except for disagreeing with the FDA on the question of people whose jobs are more likely to expose them to COVID, such as health care workers and teachers.
The committee said that these people should not yet be allowed to receive an extra Pfizer dose, but stressed that its recommendations could change if new evidence shows more people need a booster. But CDC Director Dr. Rochelle Walensky ultimately chose not to follow the advisory panel's judgement on the issue of boosters and high-risk jobs.
How did the thinking on booster shots change?
Even before the FDA's advisory panel delivered their judgement on the Pfizer vaccine, the FDA's own scientists were expressing their skepticism about the need for booster shots.
They said that "data indicates that currently US-licensed or authorized COVID-19 vaccines still afford protection against severe COVID-19 disease and death in the United States." As Matthew Herper and Helen Branswell wrote for STAT, an online publication covering health, medicine and scientific discovery news:
"On one side are drug companies and some researchers, who point to data showing the efficacy of the vaccines to protect all infections is waning and that a third shot will provide additional protection.
"On the other are those who point out that these vaccines are still keeping people out of the hospital and preventing them from dying, indicating that a booster is not needed yet."
Remember, the FDA panel's vote specifically related to whether a third shot of the Pfizer vaccine is necessary for most people. In voting against the plan, the panel was not saying the vaccine itself is unsafe, and was certainly not trying to cast any doubt on the general efficacy of the vaccines.
To reiterate, yet again, the COVID-19 vaccines work! And while breakthrough cases in vaccinated people do happen, the vaccines vastly reduce the risk of hospitalization or death. If you haven't got your first shots yet, here's how to find a COVID-19 vaccine near you.
Does this mean boosters won't happen for the general public at all?
We just don't know right now.
On Monday, the White House's chief medical adviser, Dr. Anthony Fauci, told NPR that he expected more data to become available in the next few weeks that would "actually modify and expand the recommendation" for the use of boosters to more people. "But for now we'll go with what the FDA advisory committee has recommended," Fauci said.

