“It’s heartbreaking. And it eats on me day after day after day,” Plumley said. “What Kaiser simply needs to do is hire more clinicians.”
But Kaiser says there just aren’t enough out there. The integrated health system currently has 300 open clinical positions it is trying to fill, according to a statement from Yener Balan, Kaiser’s Northern California vice president of behavioral health. Even hiring more clinicians won’t solve the problem, Balan said, adding, “We all must reimagine our approach to the existing national model of care.”
Kaiser lodged formal concerns about the bill when it was first introduced, and the trade group representing insurers throughout the state, the California Association of Health Plans (CAHP), formally opposed the bill, saying a shortage of therapists would make it too difficult to meet the two-week mandate.
“The COVID-19 pandemic has only exacerbated this workforce shortage, and demand for these services [has] significantly increased,” said CAHP lobbyist Jedd Hampton at a state Senate hearing for the bill last spring, citing a UCLA study that predicted California would have nearly 30% fewer therapists than needed to meet demand by 2028. “Simply put, mandating increased frequency of appointments without addressing the underlying workforce shortage will not lead to increased quality of care.”
But lawmakers pushed back and accused insurers of overstating the shortage. If insurers want to attract more therapists to their networks, the responsibility is on them to pay better rates and reduce administrative burdens, said state Sen. Connie Leyva, D-Chino. And if insurers want more young people to enter the mental health care profession, they have to improve the salaries and working conditions of the field now, said state Sen. Richard Pan, D-Sacramento.
As bipartisan support for the bill grew, insurers withdrew their opposition. The bill passed the Legislature with 111 lawmakers voting for it and one voting against.
“COVID, and the fact that every single one of us has been impacted significantly in terms of our isolation, I believe, has made legislators’ focus, and their understanding of the importance of treatment, almost universal,” said Julie Snyder, government affairs director for the Steinberg Institute, a supporter of the bill.
The bill itself, which would take effect in July 2022 if signed by the governor, is a solid step forward toward improving access to mental health care, with communities of color standing to benefit the most, said Lonnie Snowden, professor of health policy and management at UC Berkeley.
African Americans, Asian Americans and Latinos face the most barriers getting into care, he said, and when people of color do come in for treatment, there is a high discontinuation rate.
“So anything you can do to speed up people’s future appointments is probably going to disproportionately benefit people who are already staying away because of barriers,” Snowden said. “If you can remove one of the barriers, they’re the ones who stand to benefit.”
But there has to be some form of oversight and enforcement for the new rules to work, said Keith Humphreys, a psychiatry professor at Stanford University. Kaiser has data systems that can track the time between appointments, but other insurers contract with therapists in private practice, who manage their own caseloads and schedules.
“Who would keep track of whether people who’ve been seen once were seen again in 10 days when it’s hard enough just to keep track of how many providers we have and who they are seeing?” he said. “And if someone wasn’t seen again in 10 days, how do we tell the cases when they were denied care they wanted versus the cases where they decided one appointment is all they wanted?”
These are questions that will fall to state regulators, the California Department of Managed Health Care and the Department of Insurance.
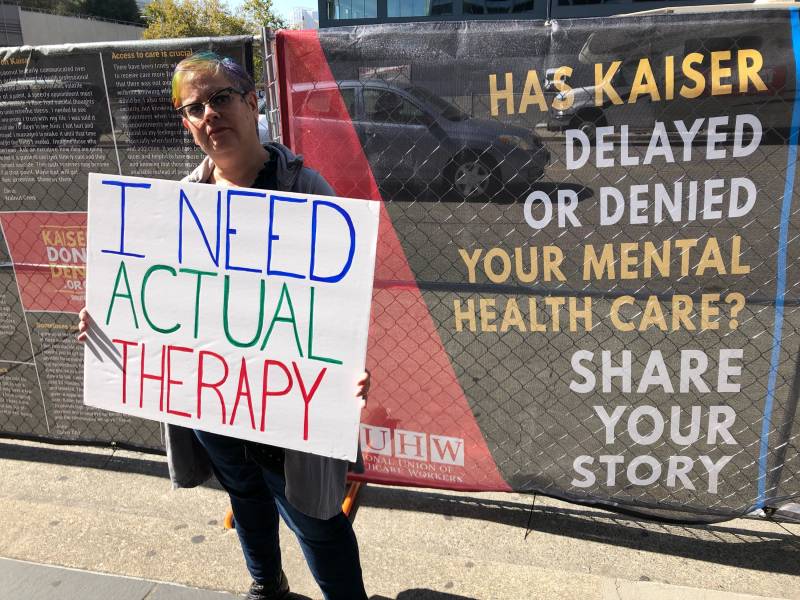
Regardless, Greta Christina says she is desperate for the bill to become law. She’s thought about looking for a new therapist outside Kaiser so she can be seen more frequently. But she really likes her therapist. She says it’s too hard to think of starting over with someone new while she’s in the middle of a cancer crisis. So she has decided to wait.
“Knowing that this bill is on the horizon has been helping me hang on,” she said.