In December 2020, KQED’s Forum interviewed four health workers experiencing the front lines of the COVID crisis in California. At the time, cases were surging in California, and no coronavirus vaccines were yet available.
Nine months later, Forum’s Mina Kim spoke with the same four health workers about the changes they have seen, and the challenges they have faced in the last year.
Read on for the highlights of their conversation.
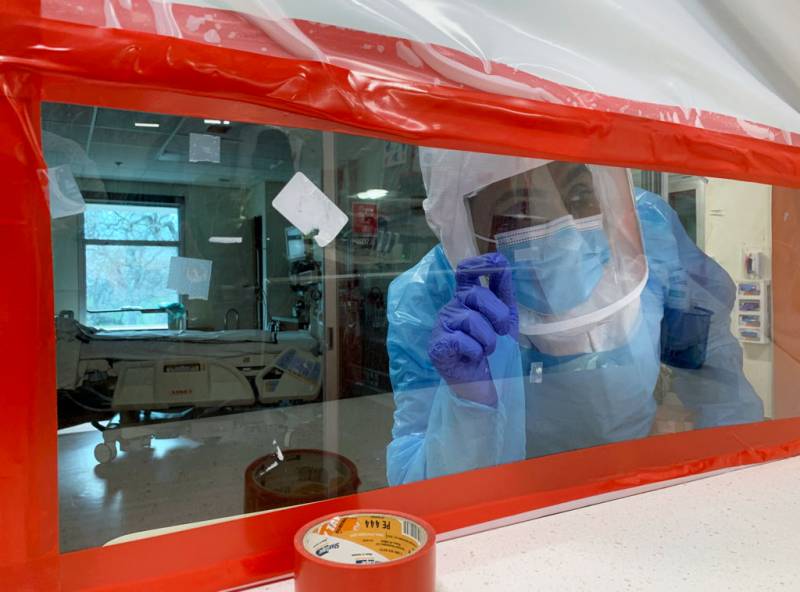
A glimpse inside our hospitals
Amy Arlund, a registered nurse at Kaiser Permanente Fresno Medical Center, noted that the dire capacity levels in her facility’s ICU experienced in the winter of 2020 had only gotten worse.
In December of 2020, said Arlund, “my ICU was at 100% capacity. I have a 12-bed ICU.”
“Here we are nine months later, my ICU is at 200% capacity. We’ve tried to divert patients to other hospitals, but unfortunately, there are no ICU beds available in the Central Valley for about a four-hour drive radius from here,” she said.
The overflow of patients in the Kaiser Permanente Fresno Medical Center has led to holding patients in the emergency room for days, and “patients who are in cardiac arrest on the regular floors,” said Dr. Parimal Bharucha, a pulmonary critical care specialist for Dignity Health in the Sacramento area.
Dr. Alex McDonald, a family medicine specialist at Kaiser Permanente Fontana Medical Center in San Bernardino County, emphasized the importance of getting a flu shot to prevent a flu surge “on top of our already covered [COVID] surge.”
“For the first surge, people [had] a fear of COVID,” said Mawata Kamara, a registered nurse at Alameda Health System’s San Leandro Hospital. “But now it seems like everybody’s out, everybody is over the pandemic.” However, there are still patients who come into medical centers and ERs with symptoms of COVID and refuse to get vaccinated, she said.
‘We are the targets’
Conversations with patients about COVID have not gotten easier in the past nine months, say the health care workers who spoke with Forum.
Medical and health professionals are “contending with misinformation about the vaccine” being spread online and through social media, said Kaiser Permanente Fresno Medical Center’s Arlund, who noted that she lives and works “in a conservative part of the central San Joaquin Valley.”