The case in southwest Louisiana was detected during routine flu surveillance and eventually sent to the CDC for confirmation. The case doesn’t change the CDC’s assessment that the risk to the general public remains low.
Still, the hospitalization is a reminder that bird flu has a well-established history of leading to severe illness and death over the past 20 years in other countries, Dr. Demetre Daskalakis with the CDC, told reporters on Wednesday during a press call.
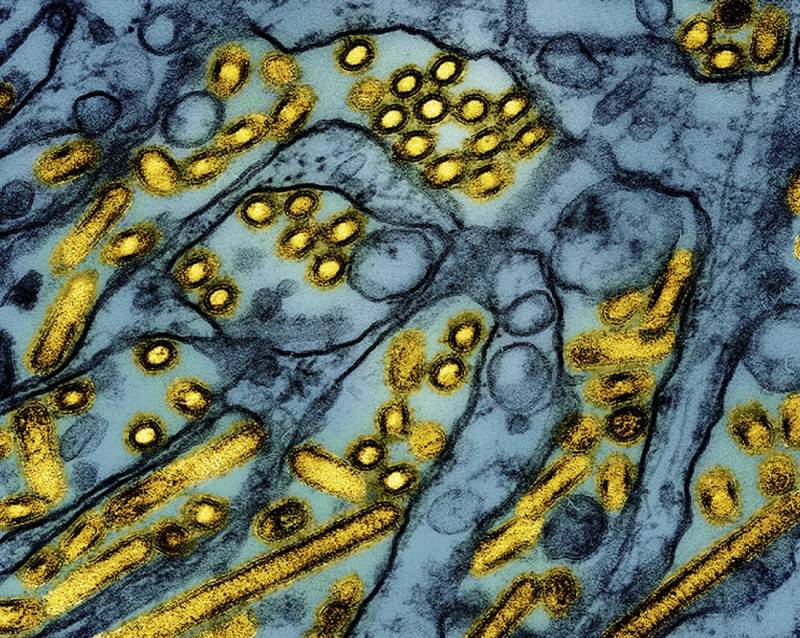
Daskalakis said his agency is doing additional sequencing to look for any worrying changes in the virus that could signal it’s evolving to better infect humans or cause more severe disease.
Scientists were concerned that the case in British Columbia exhibited certain mutations that could spell trouble, although more research was needed to understand the exact implications.
Daskalakis referred reporters to Louisiana officials conducting the investigation into the case for further details on how the person caught the virus and their symptoms.
As with the Louisiana infection, most cases have been linked back to some kind of exposure to sick animals. Dairy cattle harbor high loads of virus in their milk and that’s suspected to be causing infections in farm workers. Those working with infected poultry can also catch the virus.
However, several cases have cropped up in the U.S. that can’t be tracked back to infected farm animals, including in California and Missouri.
“Infections without a clear source of exposure do occur; neither these cases nor the cases with known animal or animal products exposure have resulted in human-to-human transmission,” Daskalakis said.