The nine Bay Area counties are in the process of incrementally reopening businesses and activities that were shut down to slow the spread of the coronavirus.
Now, with hospitalizations and deaths for COVID-19 having plateaued throughout the region, Napa, Solano and Sonoma counties are loosening restrictions according to the state’s road map, while Alameda, Contra Costa, Marin, San Francisco, San Mateo and Santa Clara counties are taking a more deliberate approach. You can see the current reopening status of all the counties here.
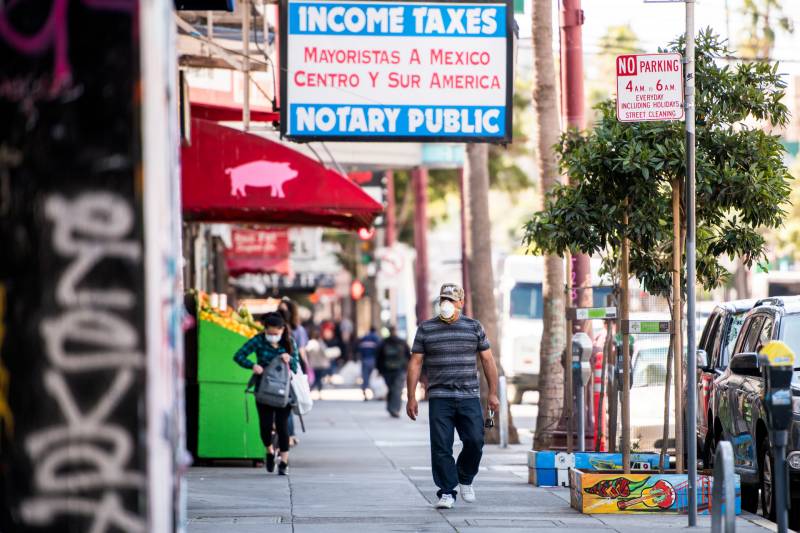
But no matter which county you live in, the fact is there are now more people interacting with each other than at any time since the Bay Area basically closed up shop in March, which by definition provides more opportunities for the virus to spread.
To get an epidemiological take on what to expect, we asked infectious disease and medical experts from UCSF, Stanford and UC Berkeley what these reopenings could mean for the Bay Area and what health officials should watch for as they grapple with the possibility of having to reinstate closures.
Dr. Yvonne Maldonado, professor of pediatrics, epidemiology and population health at Stanford University School of Medicine
‘(W)e’re just not seeing transmissions if people just wear surgical masks.’
Maldonado says, in effect, that there’s no free lunch.
“I fully expect to see additional cases,” she said. “I don’t think that the counties are going to be able to stop that, because, frankly, I think people are just really tired of being cooped up. It’s tough. And not only that, it’s tough on the economy. People want to get back to their jobs.”
But limiting the increase of new cases will be a function of how well people adhere to social distancing and prevention rules, she says. This may be difficult, given the psychological and economic toll on people that staying at home for such a long period of time has taken.
She said officials need to help businesses “enforce what they can.”
“I think the vast majority of the businesses are doing the best they can,” she said. “But we also need the public to cooperate and behave properly so that they can also reduce transmission.”
Limiting the number of people inside businesses, keeping workers and customers spaced out, and reducing “touch opportunities,” as some restaurants have done with app-based menus, will help reduce spread of the virus, she says. Basic guidelines to wear masks, wash hands and stay six feet apart are still best practices.
“What I’ve seen in the hospital is we’re just not seeing transmissions if people just wear surgical masks. I’m not talking about N95 or hazmat suits,” Maldonado said. “So if we could just do something simple, like wear a face mask, wash our hands and just stay a little bit apart, I think we can still go out. And then people can maintain their sanity and the economy, and we can still get to zero [transmissions] at some point. It won’t happen overnight, but we will get there.”
Maldonado says if an uptick in cases is observed, public county health officials will need to rethink their reopening strategy. But barring huge increases, she says, this doesn’t necessarily mean that restrictions should be reinstated.
“You give something, people are excited. If you take it back, that’s going to be tough,” Maldonado said. “I’m more worried now about people just getting so overwhelmed by this that they’re just going to stop doing everything.”
Instead of tightening back up if cases get out of hand, Maldonado recommends better enforcement of social distancing policies. Drawing circles on the grass in parks where individual households can gather while maintaining distance from others is one example, with authorities enforcing those rules.
Ultimately, she says officials need to find ways to make it easier for people to comply with directives.
“Active prevention is easier to comply with than passive, meaning when you tell people how to behave, that doesn’t work as well. So how do we put those guardrails up in ways that we can still get ourselves moving? And I think that’s where we have to be creative in our solutions, and that’s where the county health departments are really going to have to try to work on it.”
Dr. Art Reingold, professor of epidemiology at the UC Berkeley School of Public Health
”(I)t’s going to be a really difficult political and social and public health decision … to say ‘things are getting bad again, we need to reimpose X, Y and Z.’
Reingold says making predictions about potential spikes in COVID-19 cases is difficult because of two big unknowns. One uncertainty is whether the warmer summer temperatures will stall the virus to some degree; the other is whether people will continue to observe social distancing and hygiene guidelines.
“If they interpret the loosening of restrictions as license to go back to the way things used to be, I am concerned that we will see substantial resurgence, but I hope that’s not the case,” he said. “It’ll be a lot easier to answer that question in a month or two.”
He expects the virus will continue to circulate in the region for the foreseeable future, along with the same range in the severity of cases from asymptomatic to fatal. Herd immunity, which in the case of the novel coronavirus would require about 70% to 80% of the population to be vaccinated or have developed biological protection from an earlier infection, is still a long way off, he says. Scientists have estimated the percentage of the Bay Area population that’s been infected is 5% or less.
Reingold says the decision to reinstate more rigid restrictions will be informed by clinical and public health data, but he suspects there will be pressure on officials to keep things open, making tightening back up a last resort.
“I think it’s going to be a really difficult political and social and public health decision for a county or city or state to say ‘things are getting bad again, we need to reimpose X, Y and Z.’ I think that’ll be challenged both by political concerns and pushback from people.”
Dr. John Swartzberg, clinical professor emeritus at UC Berkeley School of Public Health in the Division of Infectious Diseases
‘Three steps forward, one back; three steps forward, two back. … That’s the way I think to proceed.’
Swartzberg said the safe way to open up is to “meticulously” track the numbers of positive tests.
“If you’re starting to see the trend go up, pull back. And you don’t have to pull all the way back. Follow the numbers and if the numbers drop down again, then you can let people go back to work,” he said. “The way to preserve as many lives as we can during the pandemic is to have little ripples as opposed to big waves.”
He thinks a stop-and-start approach when it comes to restrictions is the best way for public health officials to keep new transmissions in check.
“Three steps forward, one back; three steps forward, two back; three steps forward, none back; and then three more steps forward. That’s the way I think to proceed. But it’s predicated upon adequate testing because otherwise we’re flying blind.”
Swartzberg says the more testing administered on a daily basis, the more accurate the numbers will be.
“You want to get a representative sample of your community and test those on a daily basis,” he said. He thinks the state’s benchmark of 100 tests per 200,000 residents is a reasonable ratio.
He agrees with other experts that the level of adherence to social distancing and hygiene rules will determine how much cases will spike as countries reopen. This applies to the recent protests related to the killing of George Floyd in Minnesota that have attracted large crowds of demonstrators throughout the Bay Area.
“I’m very concerned, not about why people are protesting, but about how,” he said in email. “Without social distancing, without wearing masks and with raised voices (and, therefore, lots of droplets in the air), the virus is likely to spread. And, it’s not just the protesters, but also the police who are not wearing a mask.”
Swartzberg says it could take three weeks for the consequences of so many people gathering together without protection to manifest.
Dr. Bob Wachter, chair of the Department of Medicine at UCSF
‘There’s every reason to believe we’ll see an uptick in cases.’
With no vaccine and only about 1% to 5% of people in the Bay Area estimated to have been infected with SARS-CoV-2, Wachter says the vast majority of the population is still susceptible. And for those who did have the virus, whether they have lasting protection from antibodies is still being determined. Wachter says that means reopenings will likely result in an uptick in cases.
“If you believe, as I do, that the reason that the Bay Area was hit so mildly over the last few months is the behavior of our people in terms of distancing and mask wearing and staying home, then if we lighten that up, there’s every reason to believe that we’ll see an increased number of new cases,” Wachter said.
“We’re in that very tricky phase where loosening up a little bit is appropriate, as long as we’re watching very carefully and as long as we are ready to tighten things back up again if things start getting out of hand.”
In terms of the recent Bay Area protests, Wachter said mask-wearing is critical. “Large crowds with people shouting is a formula for spread if people aren’t wearing masks. If they are and are doing their best to keep a distance from others, it is safe enough that people should make their own choices. I completely understand the motivation for protesting and people should just do it as safely as they can.”
Wachter says making the call to reinstate lockdowns will be a difficult one for officials to make, and waiting for hospitalizations or deaths to rise may come too late to contain a surge.
“If those are your main signals, those are picking up things that happened two weeks ago,” he said. “If I were to catch COVID today in the supermarket, I feel fine for on average five days. If I was destined to get really sick, that would probably take another five to seven days. And if I was destined to go to an ICU or to die of it, it would probably take another week or two. So those are really late signals.”
Wachter says widespread testing is needed to detect small blips in cases before a large surge occurs. He also says the number of calls to hospitals and urgent care centers from people with symptoms could be an early indicator for a wave of new cases.
“The analogy I use is if you were in New York in March, you were in the middle of a wildfire. In San Francisco, in the Bay Area … there’s no wildfire. But there are embers. And we have to figure out ways of finding those embers and quickly containing them. And that means a lot of testing. It means anybody with any symptoms at all gets in for rapid testing. If they’re positive, we go ahead and find their contacts, we test them. We’re also doing some testing [at UCSF] of asymptomatic people, because we know a lot of people with the virus won’t have symptoms, to try to pick up the early warning signs that there is COVID in the community.”
Wachter says if cases start to increase, dialing back on reopening is advisable. But to what degree could depend on where in the community the cases are coming from. If surges are traced to religious services or other activities, Wachter says closures could be tailored accordingly.
“In March, we didn’t have that kind of information. So the prudent thing to do was to shut down everything. But now I think we’ll be able to be a little bit more pinpoint about it. That said, if truly we had a doubling of cases, I would go back to March. I would say it’s time to shut back down everything.”