Buckling Up
Passing safety laws and getting people to embrace them can take years or even decades. While it’s standard practice now for us to buckle up before pulling out of the driveway, modern automobile seat belts weren’t invented until the 1950s, a half-century after Ford brought motorcars to the masses with the Model T. The idea for retractable belts in passenger cars is credited to a neurologist in Pasadena, who’d been treating a large number of patients suffering from head traumas sustained in car crashes.
But the U.S. didn’t require car manufacturers to equip vehicles with seat belts until1968. Even then, no law required passengers to wear them. That occurred in the 1980s, when states began mandating people to buckle up or risk a fine.
With COVID-19, Swartzberg says, we can’t afford that long of an adjustment period; people have to embrace harm reduction now to keep the virus from spreading. Most public health officials agree that the lack of consistent messaging from federal leadership about the efficacy of these practices has been a major barrier to fighting the pandemic in the U.S. For example, a recently released study by Cornell University researchers found that President Trump is “likely the largest driver” of COVID-19 misinformation.
Secondhand Smoke
Some health experts say the lessons learned from anti-tobacco campaigns show that certain strategies may be more effective than others at changing people’s behavior.
Dr. Richard Jackson, professor emeritus at the UCLA Fielding School of Public Health and a former state of California public health officer, says getting to the point where bans were enacted on smoking in public spaces like restaurants, planes and parks took years. What eventually tipped the scales for lawmakers and the American public, Jackson says, was not the message that smoking is bad for you, but rather that lighting up can harm other people.
“It was when we showed that flight attendants were actually getting sick from being in a confined space with a lot of smokers, that was the beginning,” Jackson said. “But eventually, over time, it led to the ban of indoor smoking.”
It wasn’t until 1995 that California paved the way for smoking bans when it became the first state to outlaw smoking in indoor workplaces.
Behavioral economists have a name for actions that affect not ourselves but other people or the whole of society: externalities.
Mask wearing can reduce the externalities of leaving your house during the COVID-19 pandemic because studies show that it helps prevent virus transmission to other people, who may not even know they’re contagious.
When it comes to choosing not to wear a mask, Jackson says, a person might argue: “It’s my life, I can take that risk.” But helping them understand that flaunting this precaution can endanger a child, a loved one, an innocent bystander — what Jackson calls “sympathetic victims” — may encourage holdouts to think twice about ignoring public health orders.
Cultural Differences
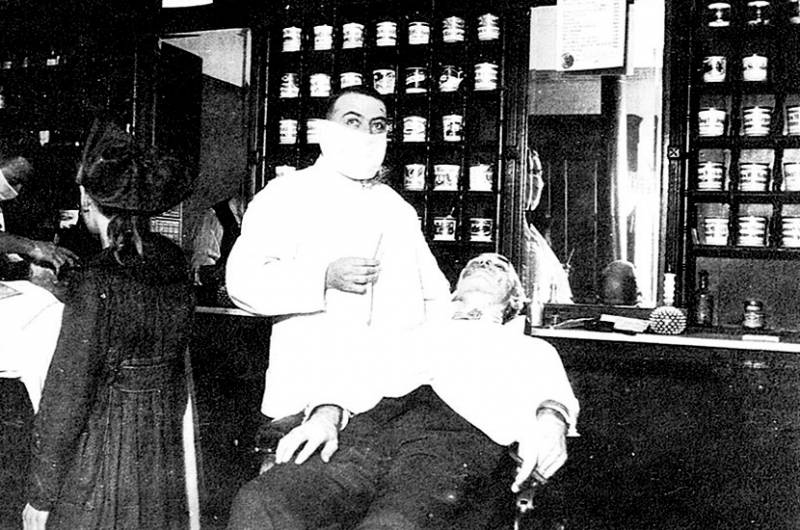
The coronavirus pandemic isn’t the first time Americans have been asked to pull masks over their faces, avoid crowds, and subject themselves to a shutdown of parts of the economy to fight a deadly virus.
Doctors prescribed a strikingly similar regimen to fight the 1918 Spanish influenza pandemic, says Dr. Lee Riley, head of the infectious disease and vaccinology division at the UC Berkeley School of Public Health. An estimated 50 million people worldwide and 675,000 in the U.S. died from complications caused by the virus, according to the U.S. Centers for Disease Control and Prevention.
“If you look at some pictures from that period, a lot of people were wearing masks,” Riley said. “They washed their hands, kept social distance, and local governments tried to make sure that people didn’t congregate in large numbers, everything that they’re saying right now.”
Studies suggest public health measures reduced the 1918 flu pandemic up to 50 % in some cities where they were implemented early on.
“That was a big pandemic, almost two years,” Riley said, “And eventually this virus petered out. So the public health measures work.” He added that the pandemic was contained long before the first approved flu vaccine, which was developed in the 1940s.
Riley points out that wearing masks to thwart disease has become the social norm in some countries around the world, particularly in Asia. He grew up in Japan in the 1950s and remembers wearing a mask to elementary school.
Because reliable vaccines to fight influenza or bacterial respiratory diseases didn’t yet exist, wearing a mask was the primary way people kept from getting sick, Riley says. But there was also a cultural incentive.
“There’s a phrase in Japan that was instilled in all little kids: Never cause harm to strangers and your neighbors,” he said. “And so one major driving force why people will wear a mask is not just to protect themselves, but also (to) prevent the transmission.”
Japan, Riley said, is a more socially conscious culture when compared with more individualistic societies in the West. When it comes to fighting the pandemic, he says the U.S. could benefit from this baked-in harm reduction philosophy.
“I think, you know, Americans are not that different from other people when they start really thinking about this.” he said. “And when we have a good leadership model, we can really serve as a model.”
Jon Brooks contributed to this report.