A key provision aims to prevent investors from meddling in health care decisions, ensuring physicians and medical professionals retain autonomy over patient care.
Still, private equity firms would have the right to challenge the state’s decisions in court if they believe regulatory actions are unjustified.
Consumer advocates, labor unions, and the California Medical Association call the measure crucial to patient care.
However, it faces fierce opposition from industry and business groups who worry that the oversight will deter critical funding streams.
The American Investment Council argues that further regulation could discourage investment in health care and limit innovation and access to capital. The California Hospital Association also opposes it, warning that the bill could create additional hurdles for much-needed investments in the state’s health care infrastructure, especially as hospitals face staffing shortages and capacity constraints.
Venture-backed digital health companies worry that companies will struggle to gain traction under the new regulation.
Why is legislation needed?
Private equity investment in health care nationally increased from $5 billion annually in 2000 to $100 billion in 2018.
“Health care is a very durable industry,” Cai said. “It’s viewed as a stable investment, with ample opportunities to consolidate fragmented outpatient clinics and hospitals.”
Physician practices are particularly appealing targets, with the number of transactions increasing sixfold over the past decade, frequently resulting in notable hikes in patient costs.
The market appeal is clear: more efficient management can streamline costs, and with an aging population of baby boomers, demand for health care services is expected to soar. “Because of these factors, private equity’s presence in health care has more than tripled in the last decade or so,” Cai added.
This influx of capital has stirred alarm among policymakers and patient advocates, who argue that profit-driven investors prioritize financial returns over patient care. Private equity firms ultimately need to make returns and protect their companies against potential risks — for them, it can’t just be about mission.
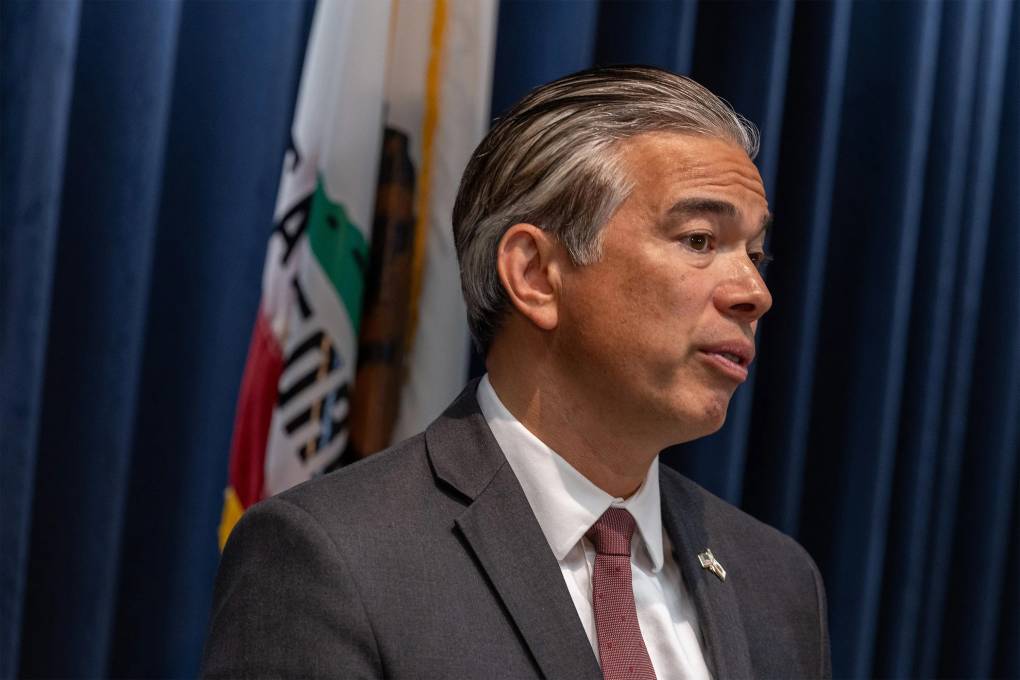
“Who is reviewing these transactions to ensure they serve the public interest?” asked Assemblymember Jim Wood (D-Healdsburg), the bill’s sponsor in a recent press release. “No one is, because all of these transactions are happening under the radar.”
Studies reveal alarming outcomes
The impact of private equity ownership is particularly pronounced in long-term care settings. One study found that mortality rates in nursing homes rose by a jaw dropping 11% after private equity firms took over. Patient mobility decreased, and the use of antipsychotic medications may have increased.
“We rarely see increases like that after any kind of change,” Cai noted. “That study was an earthquake for the industry.” In response, Federal health officials required nursing homes to reveal if they’re owned by private equity firms. Starting in 2026 the facilities must increase staff to ensure each patient receives more attention.
A separate study, published in the Journal of the American Medical Association, found a 25% increase in adverse events—such as falls and surgical infections—after hospitals were bought by private equity firms. A systematic review of available research shows that private equity ownership does not typically benefit patients and, in extreme cases, may lead to the closure of facilities, particularly in rural or underserved areas where profit margins are slim.