If mpox cases are still very low, why is SFPDH recommending awareness? One big reason: The city’s Pride celebrations are just around the corner in June, and it’s a time when many folks are gathering and also arriving into the region from other parts of the United States, says Cohen.
“Last year we saw that the mpox outbreak really was fueled during the spring and summer season,” Cohen said, “and we think that that was largely related to a lot more travel — as well as large gatherings — with many people coming together from different parts of the country, and the world.” In the realm of infectious diseases, Cohen said, that’s “a time when things can spread more quickly.”
Another reason: Last year’s mpox outbreak starting in the spring and the summer makes public health officials think that “it’s also possible there is a seasonal nature to mpox,” said Cohen — as there is with many viruses. “There’s a lot we still are learning about mpox.”
Who is most at risk?
SFDPH says that the 2022 mpox outbreak predominantly affected communities of gay and bisexual men, and men who have sex with men (MSM), as well as trans and nonbinary people who have sex with men.
This 2022 outbreak was “unique compared to what had been known about mpox previously,” said Cohen, because the virus “really seemed to spread through sexual transmission, and [was] associated with sexual activities.” Read more about how mpox spreads.
“When you look at our national data, almost 97% of cases in the U.S. were in people who are cis men,” said Cohen. “There were very, very few cases in cisgender women and also very few cases — about 0.08% — in children under the age of 16.”
Should I get the mpox vaccine?
The mpox is a two-dose vaccine series, with roughly a month between doses. So …
If you got both doses of the mpox vaccine in 2022:
You’re all up to date — and you don’t need to get another mpox vaccine in 2023. There’s no recommendation at this time to get an mpox booster, says Cohen.
If you didn’t get the mpox vaccine in 2022:
Go ahead and get your first dose as soon as possible, and get your second dose around 28 days later. A good reason to move quickly to get your first dose: “If you receive your first dose on May 13, you will be eligible for your second dose by the Saturday, June 10 event and will receive maximum immunity before Pride,” stated SFDPH in a recent statement regarding an upcoming mpox vaccination event taking place in San Francisco on Saturday, May 13.
If you got only your first dose of the mpox vaccine in 2022, or more than 28 days ago:
Get your second dose as soon as possible, says Cohen. “Getting both doses of the vaccine is very critical for protection,” she said.
Reminder: The mpox vaccine is available for everyone.
In 2022 public health officials were originally only offering vaccines to people who’d been exposed to mpox, or were categorized as being in a specific group more at risk from mpox. Those eligibility criteria are no longer in effect, and anyone who wants an mpox vaccine can get one in San Francisco, and in many other areas of California.
“Right now there are no limitations on supply,” said Cohen. “So I think that that is really going to help us with our response this summer.”
Where can I find the mpox vaccine?
Your mpox vaccine will be 100% free, and you don’t need health insurance to receive one. As with the COVID vaccine, receiving an mpox vaccine won’t make you a public charge or affect any future immigration processes you may enter into, and you won’t be asked about your immigration status to receive the mpox vaccine.
You can schedule an appointment for an mpox vaccine, or choose a walk-in clinic.
If you live in or near San Francisco:
To be fully vaccinated against mpox in time for Pride, SFDPH recommends going to this weekend’s vaccination event, held in partnership with Folsom Street Events and the Leather and LGBTQ Cultural District. First and second doses of the mpox vaccine will be available at the May and June SOMA Second Saturday events:
Dates: Saturday, May 13 and Saturday, June 10
Location: 12th Street between Folsom and Harrison streets
Time: 12 p.m. to 5 p.m.
See a full list of mpox vaccine sites near you in San Francisco. Cohen confirms that you don’t have to be a city resident to get vaccinated for mpox in San Francisco.
Mpox vaccination sites elsewhere in the Bay Area and California:
How effective is the mpox vaccine?
“We’re still learning about the durability of protection after a vaccine or after [an mpox] infection itself,” said Cohen. No vaccine is 100% effective, she stresses, and the mpox vaccine is no exception — but several analyses by the CDC show that “it looks like it provides about 69% reduction in risk with the full two dose series.” So while protection from mpox isn’t 100%, it’s still “really good protection,” said Cohen.
Another reason to get an mpox vaccine: It could help reduce your symptoms — which can be painful — if you do still get infected, said Cohen.
“That’s, of course, really a good outcome of the vaccine — because we did see some pretty severe cases of mpox last summer in unvaccinated individuals,” said Cohen. “And we really don’t want people to experience the distressing and painful symptoms that occurred at the same time.”
What you need to know about mpox
How does mpox spread?
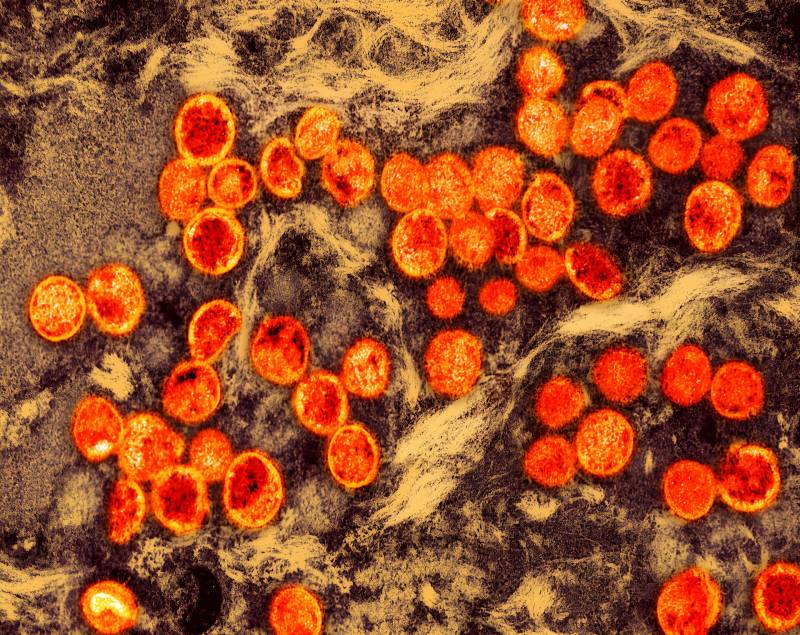
Mpox is a disease that is caused when a person is infected with the mpox virus. As the name might suggest, the virus is related to the smallpox virus but is generally less severe and “much less contagious” than smallpox, according to CDPH.
Mpox spreads through “prolonged skin to skin contact,” says SFDPH, which can include sex, kissing and sharing bedding or clothing.
What are the symptoms of mpox?
The symptoms of mpox often start as flu-like symptoms, says SFPDH, but the virus also appears as a rash or sores or spots that can resemble pimples or blisters on the skin anywhere on the body, especially around your genitals. These spot often start as “red, flat spots, and then become bumps,” says SFDPH, before the bumps become filled with pus, and turn into scabs when they break. See the full list of mpox symptoms from SFDPH.