Skip straight to:
For the past several weeks, advances with COVID-19 vaccines have offered hope in what has felt like an endless slog through this pandemic.
On Nov. 20, Pfizer applied for emergency use authorization for its COVID-19 vaccine from the Food and Drug Administration. On Monday, Moderna announced it would also be applying for authorization for its vaccine, which reportedly has a 94.1% efficacy rate. If approved, doses could start rolling out before the end of the year.
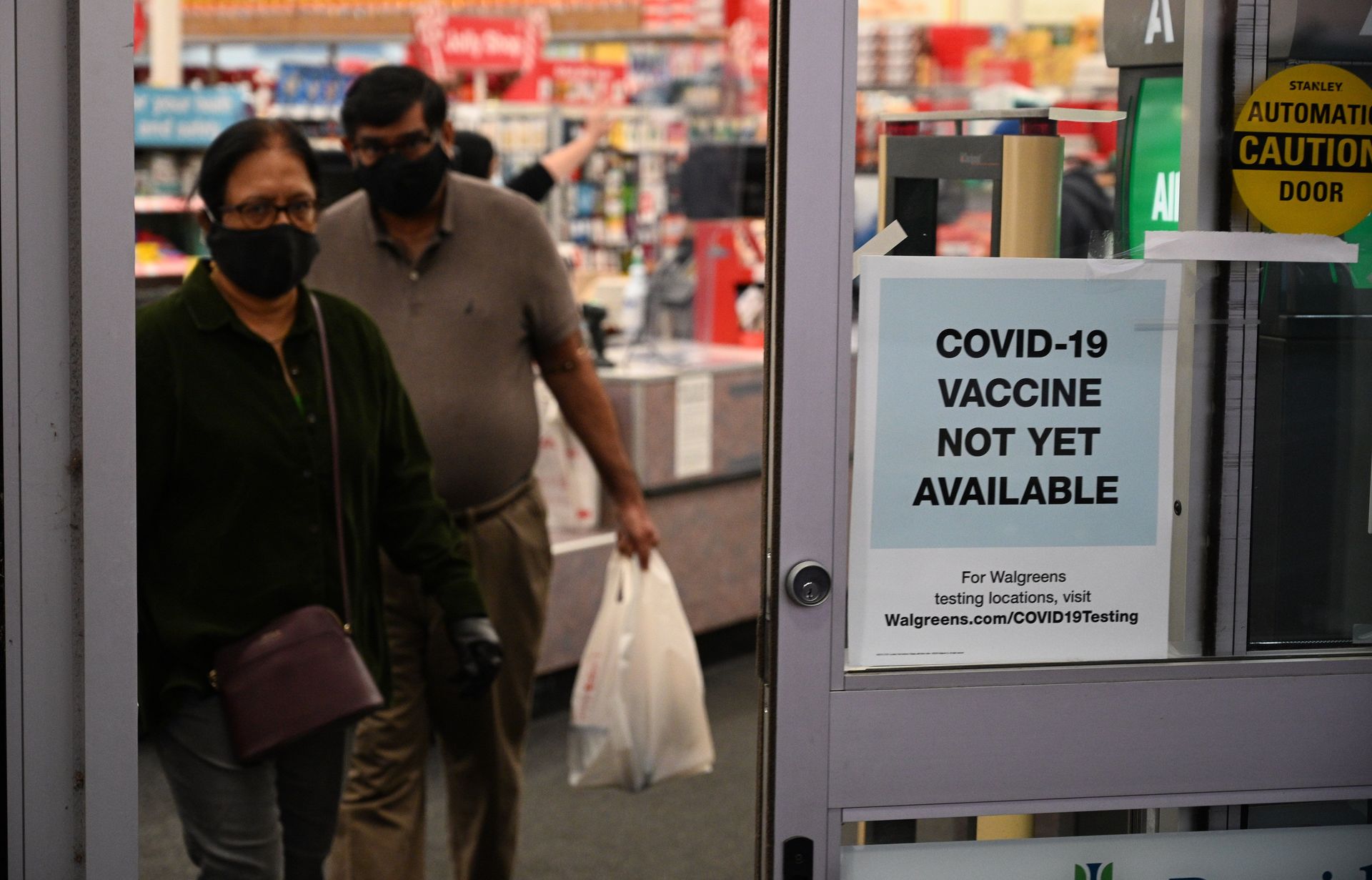
But with the possibility of a vaccine in the near future coming into clearer focus, questions are being raised how these vaccine doses might be distributed. In California, state officials have made it clear that health care workers will be the first to receive the vaccine. But since the initial rollout will likely be limited, officials will have to decide which health care workers will get the vaccine first.
What does that mean, then, for the rest of us?
KQED Forum host Michael Krasny spoke with Dr. Robert Wachter, chair of the UCSF Department of Medicine, about the vaccine rollout and when the general public should realistically expect a dose.
This interview has been edited for length and clarity. Hear the full interview
Michael Krasny: There's good news on the horizon with respect to vaccines. And I'm interested in finding out your thoughts about the timing, first of all, but also the distribution of vaccines at this point.
Robert Wachter: Let's start with the big picture: A month ago, we didn't know for sure that we would get a vaccine that worked. I mean, we've been working on an HIV vaccine for 30 years. We don't have one. So November, really, will go down in history as a remarkable month in the history of science, that now we have three vaccines that we know work — two of them remarkably effective, the AstraZeneca [vaccine] a little bit less so. But the news on the Pfizer and the Moderna vaccine are breathtaking, really beyond anything any of us had anticipated.
But even more impressively, the Moderna news that came out this morning in their trial: There were 30 severe cases, 30 patients that were quite sick that had to go to the hospital or to the ICU or had very low oxygen. All of them — all 30 — were people that got the placebo. Zero of them were in people that got the vaccine. So these are breathtakingly effective.